Dear Sir:
Cervical artery dissection in young adults accounts for 10% to 25% of all ischemic strokes. Sample size is one of the foremost limitations delineated in a majority of the studies evaluating recurrent risk of stroke due to cervical artery dissection [1].
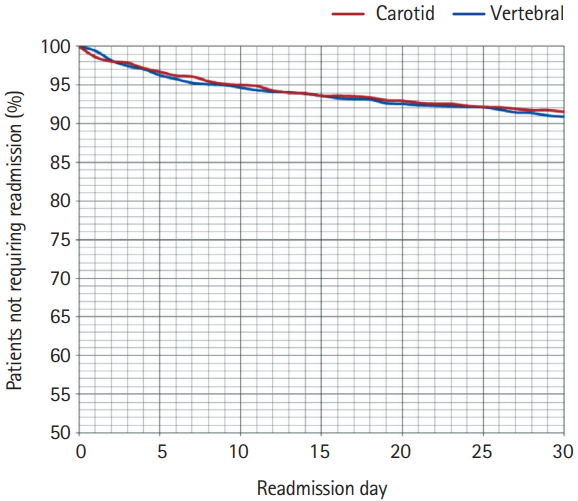
We used the 2014 Nationwide Readmission Database to analyze 30-day unplanned readmissions (30RR) for symptomatic carotid artery dissection (SCAD) (weighted n=2,686) and symptomatic vertebral artery dissection (SVAD) (weighted n=2,837) [2]. Differences in demographic characteristics of both the groups based on the relevant available variables in the database and International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes are described in Table 1. Readmission trends are depicted in Figure 1. Top causes of unplanned readmissions are described in Table 2.
Overall 30RR for SCAD was not significantly higher than SVAD (9.08% vs. 8.43%, P=0.412). Overall unplanned readmissions due to ischemic strokes in our study are similar to the findings of the CADISS trial1; however, 30RR due to ischemic stroke were higher in SVAD compared to SCAD (4.14% vs. 1.60%, P<0.001). Approximately 50% of total readmissions for first 30 days were admitted by day 7 in both SCAD and SVAD groups [3,4].
Higher incidence of intracranial dissection with SVAD compared to SCAD potentially explains higher intracranial hemorrhage with SVAD (intracerebral hemorrhage: 11.62% vs. 5.41%, P<0.001; subarachnoid hemorrhage: 3.21% vs. 0.78%, P<0.001) [5]. The incidence of intracerebral hemorrhage amongst readmitted patients was also significantly higher with SVAD (7.9943% vs. 3.6257%, P=0.016). These findings are less likely to be related to reperfusion therapies, as anterior circulation infarcts tend to have higher hemorrhagic transformation rates [6]. We also noted a higher incidence of reperfusion therapies with carotid dissections.
Peripheral, visceral and aortic artery aneurysms were present in 11.55% patients with SCAD (related 30RR 1.16%, third leading cause) and 4.73% patients with SVAD patients (related 30RR 0.88%, second leading cause). These findings suggest that there might be some value of having a low threshold to screen these patients for additional vascular abnormalities, especially those with known connective tissue disorders.
Tertiary care centers are reported to have poorer outcomes for cervical artery dissections, as complicated cases are usually referred to such institutions [7]. Our study too showed a higher readmission trend in larger size hospitals. Medicare and Medicaid as primary payer had higher rates of readmission compared to private insurance along with length of hospital stay as described in Table 1. It is important to consider that quality of access to care after discharge from hospital could be a contributing factor leading to higher readmissions in such population.
The study findings need to be taken into consideration in light of shortcomings intrinsic to secondary analysis of a large administrative database. We were not able to identify the approach for medical management during index hospitalization (i.e., anticoagulant vs. antiplatelet therapy), imaging information, location of dissection (intra vs. extracranial), and degree of vessel stenosis. Knowledge of these point of care clinical information would certainly further help identify the root causes of differences in readmission risk.
Despite these limitations, our study represents one of the largest cohort of symptomatic cervical artery dissection cases and contributes to current understanding of primary etiologies and demographic differences of 30 days readmissions. It shows that overall readmission rates are not significantly different for SCAD and SVAD. However, patients with vertebral artery dissections have higher rates of readmission with ischemic stroke and also are more likely to have intracranial hemorrhage.