Multidisciplinary Approach to Decrease In-Hospital Delay for Stroke Thrombolysis
Article information
Abstract
Background and Purpose
Decreasing the time delay for thrombolysis, including intravenous thrombolysis (IVT) with tissue plasminogen activator and intra-arterial thrombectomy (IAT), is critical for decreasing the morbidity and mortality of patients experiencing acute stroke. We aimed to decrease the in-hospital delay for both IVT and IAT through a multidisciplinary approach that is feasible 24 h/day.
Methods
We implemented the Stroke Alert Team (SAT) on May 2, 2016, which introduced hospital-initiated ambulance prenotification and reorganized in-hospital processes. We compared the patient characteristics, time for each step of the evaluation and thrombolysis, thrombolysis rate, and post-thrombolysis intracranial hemorrhage from January 2014 to August 2016.
Results
A total of 245 patients received thrombolysis (198 before SAT; 47 after SAT). The median door-to-CT, door-to-MRI, and door-to-laboratory times decreased to 13 min, 37.5 min, and 8 min, respectively, after SAT implementation (P<0.001). The median door-to-IVT time decreased from 46 min (interquartile range [IQR] 36–57 min) to 20.5 min (IQR 15.8–32.5 min; P<0.001). The median door-to-IAT time decreased from 156 min (IQR 124.5–212.5 min) to 86.5 min (IQR 67.5–102.3 min; P<0.001). The thrombolysis rate increased from 9.8% (198/2,012) to 15.8% (47/297; P=0.002), and the post-thrombolysis radiological intracranial hemorrhage rate decreased from 12.6% (25/198) to 2.1% (1/47; P=0.035).
Conclusions
SAT significantly decreased the in-hospital delay for thrombolysis, increased thrombolysis rate, and decreased post-thrombolysis intracranial hemorrhage. Time benefits of SAT were observed for both IVT and IAT and during office hours and after-hours.
Introduction
Thrombolysis, including intravenous thrombolysis (IVT) with tissue plasminogen activator (tPA) and intra-arterial thrombectomy (IAT), is a proven therapy for patients suffering from acute ischemic stroke [1,2]. However, the benefits of thrombolysis are highly time dependent. Earlier thrombolysis is associated with decreased patient mortality and morbidity, and post-thrombolysis intracranial hemorrhage (ICH) [3,4]. Therefore, intensive efforts should be taken to decrease the time to thrombolysis for eligible stroke patients [5].
The current guidelines state that the door-to-IVT time should be within 60 min of hospital arrival [1]. A recent national quality improvement initiative in the United States was associated with improved timeliness of tPA administration [6]. Nevertheless, the goal of a door-to-IVT time within 60 min was achieved in only 40% of patients treated with IVT. A comprehensive report from Korea also reported a median door-to-IVT time of 56 min [7]. Surprisingly, the Helsinki model showed a median door-to-IVT time of only 20 min [8]. However, the success of this model was limited to IVT and was based on a province-wide centralized hospital system. The Melbourne model provided a median door-to-IVT time of 25 min, but out-of-hours delays were 62 min [9]. To date, no studies have reported a method to decrease the time delay for both IVT and IAT, and which is feasible 24 h/day.
We aimed to decrease the in-hospital delay for both IVT and IAT during both after-hours and office hours using a multidisciplinary approach. In addition, we investigated whether the reduction in time to thrombolysis was related to increases in the thrombolysis rate and decrease in the post-thrombolysis ICH rate.
Methods
Local emergency medical service system
Korea has a nationwide, local government-funded emergency medical service (EMS) system. The central EMS dispatch office can be reached on one representative phone number, and then communicates with branch EMS stations that are located closest to callers. However, the EMS does not provide a system by which emergency medical technicians (EMTs) can communicate with the receiving hospitals regarding the care of stroke patients. EMTs usually transport stroke patients to the closest general hospitals. There is no central hospital dedicated to EMS transportation of stroke patients. Therefore, 8 out of 61 EMS stations around Seoul and Gyeonggi-do were in charge of 78% of EMS transportations of stroke patients to our emergency room (ER) between 2014 and 2015.
Preexisting hospital system
At our hospital, the evaluation of a stroke, using both computed tomography (CT) and magnetic resonance imaging (MRI) technology, as well as thrombolytic therapies, has been available 24 h/day for over a decade. MRI was used for routine imaging to screen for cases of acute stroke until 2005. Because of concerns of an increasing door-to-imaging time, we adopted a noncontrast CT scan for imaging screening followed by a multimodal MRI for thrombolysis candidates in 2005 [10]. Intravenous tPA infusions were initiated in the ER and patients were subsequently transported to the MRI room. The MRI room was relocated next to the ER in 2010. The decision whether or not to perform an additional IAT was made after MRI acquisition. Our protocol for CT and MRI has been detailed previously [11,12]. A computerized physician order entry system for patients experiencing acute stroke was adopted in 2007 [13]. The time window for intravenous tPA was extended to 4.5 h in January 2014. We performed intra-arterial chemical thrombolysis until 2010; since the introduction of the Penumbra System and stentriever device to our hospital in late 2010, we have been preferentially performing IAT using these devices.
The Stroke Alert Team
We aimed to decrease the time to thrombolysis. To achieve this goal, in January 2016, we discussed a new model and organized the Stroke Alert Team (SAT), which was comprised of neurologists, emergency physicians, nurses, laboratory physicians and technicians, radiologists, intervention neuroradiologists, radiology technicians and nurses, and admission officers.
Our plan to decrease the thrombolysis time through prospective SAT activities was accepted as the Asan Medical Center Performance Improvement Project 2016. We prepared the SAT project between January 2016 and April 2016 and it was formally initiated on May 2, 2016. As we announced to hospital government and personnel and 8 branches of EMS stations in advance, our specific goals were as follows: (1) to decrease the median door-to-IVT time to 20 min, and (2) to significantly decrease the median door-to-IAT time from that of the past 2 years. We did not specify numbers for the door-to-IAT time because we could not find any references to previous studies or guidelines. We compared the SAT data with the previous data over the past 2 years to define specific goals for motivating SAT members. Moreover, there were no other changes made to the hospital system, structure, or personnel during this period. The SAT program was operational during both office hours and after-hours.
Details of our workflow for the SAT project are described in the Supplemetary Methods and are summarized as follows: (1) we identified the factors causing in-hospital delays; (2) we introduced ambulance prenotification through which EMTs could make direct calls to SAT neurologists 24 h/day; (3) we reorganized each step, including moving the patients directly to a resuscitation room in the ER, performing point-of-care tests (POCT), preparing tPA kits, injecting tPA on the CT table, and the follow-up group messages. We avoided regularly confirming routine laboratory tests, electrocardiography, and chest radiography; (4) advance notification was given to the neuroradiology intervention team. SAT neurologists sent these messages immediately after obtaining the noncontrast CT scans based on (i) NIH Stroke Scale scores (NIHSS) of 8 or more; or (ii) observation of cortical symptoms including aphasia, neglect symptoms, and eyeball deviations; and (iii) <12 h after symptom onset; and (5) real-time and regular feedback to SAT members were emphasized (Table 1, Supplementary Table 1, Supplementary Figure 1) [14].
Definitions
The stroke onset was considered to be the time at which the patient developed stroke symptoms or when the patient was last known to be without ischemic symptoms in cases of an uncertain onset time [11]. The IVT time (needle time) was defined as the time when an injection of intravenous tPA was initiated. The IAT time (puncture time) was defined as the time when the intra-arterial catheter was placed in the groin. Post-thrombolysis ICH was defined as a parenchymal hematoma (PH1 and PH2) on CT scans performed within 36 h following thrombolysis [15]. The CT scans were interpreted by two independent investigators blinded to the clinical data.
Standard protocol approvals, registrations, and patient consent
This study was approved by the institutional review board of the Asan Medical Center. The need for written informed consent from the patients was waived due to the retrospective nature of this study.
Statistical analysis
We compared the baseline characteristics of patients, time intervals between each step of the evaluation and management, thrombolysis rates, and post-thrombolysis ICH before and after SAT implementation. We used a Pearson’s chi-squared test or Fisher’s exact test for categorical variables and a Student’s t-test or Mann-Whitney U-test for continuous variables, as appropriate. The interobserver agreement for the interpretation of post-thrombolysis ICH was determined by calculating the kappa coefficient for each investigator. In addition, the baseline characteristics of the thrombolysis patients and time to thrombolysis were grouped by year from March 2005 to August 2016 for demonstrating yearly trends. Statistical significance was defined as a two-tailed P-value of <0.05. All statistical analyses were performed using SPSS version 21 (IBM Corp., Armonk, NY, USA).
Results
A total of 1,715 patients experiencing acute ischemic stroke were admitted to our hospital via the ER between January 2014 and December 2015; 297 patients between January 2016 and April 2016; and 297 patients between May 2016 and August 2016. Between January 1, 2014 and August 31, 2016, 247 out of 2,309 patients received thrombolysis for an initial diagnosis of a stroke. Data from one patient with TIA who received IVT before SAT implementation and one patient whose tPA infusion was discontinued because of the identification of an intracranial aneurysm following SAT implementation were included for further analysis. However, data from two patients with stroke mimics (one patient with conversion disorder before SAT implementation, and the other patient with Bell’s palsy after SAT implementation) who received IVT were excluded for further analysis. Thus, we performed a statistical analysis for 245 patients who received thrombolysis between two time periods: “before SAT” (from January 1, 2014 to May 1, 2016) vs. “after SAT” (from May 2, 2016 to August 31, 2016). Of the 245 patients that were included in this study, demographic features, initial NIHSS, thrombolysis types, time to each step of evaluation and thrombolysis, and post-thrombolysis ICH are presented in Table 2.
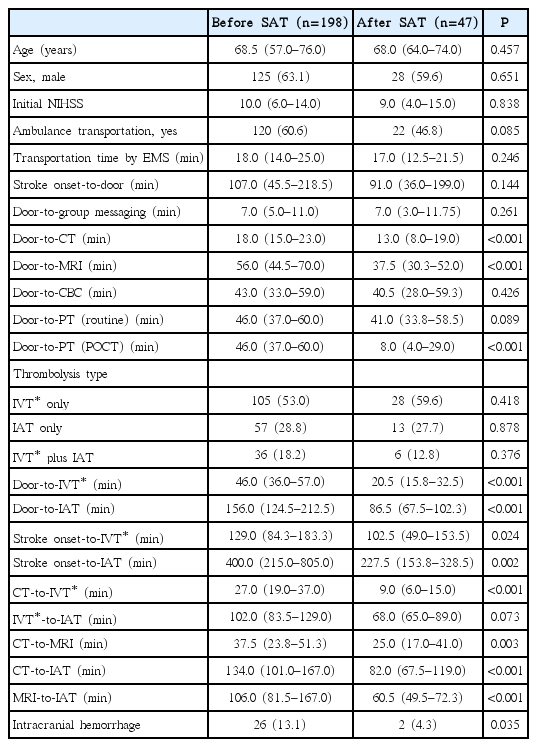
Baseline characteristics, time to evaluation, time to thrombolysis, and post-thrombolysis intracranial hemorrhage
Prehospital activities
Of the 245 thrombolysis patients, 142 (58.0%) visited our hospital by EMS. Ambulance prenotification was employed in 13 (59.1%) out of 22 EMS-transported thrombolysis patients after SAT implementation. In contrast, we received 37 prenotification calls from EMTs after SAT implementation. The final diagnoses of these 37 cases included stroke and TIA for 25 (67.6%) patients (ischemic stroke: n=20; ICH: n=4; and TIA: n=1). Of 12 nonstroke patients, SAT was activated in seven patients, but not activated in five patients despite prenotification. There were 13 (65%) out of 20 ischemic stroke patients for whom ambulance prenotification was utilized and that subsequently received thrombolysis.
The median onset-to-door time was 101 min and this did not change following SAT implementation (P=0.144). The median EMS transportation time was 18 min and did not change following SAT implementation (P= 0.246).
In-hospital activities
The median door-to-CT time decreased from 18 min to 13 min after SAT implementation (P<0.001). The median of door-to-MRI time decreased from 56 min to 37.5 min after SAT implementation (P<0.001). The median time of door-to-prothrombin time (including POCT) decreased from 46 min to 8 min after SAT implementation (P<0.001). However, the time for the reports of routine laboratory tests, including complete blood count (P=0.426) and routine prothrombin time (P=0.089), did not change significantly after SAT implementation.
The median door-to-IVT time decreased from 46 min (interquartile range [IQR] 36–57 min) to 20.5 min (IQR 15.8–32.5 min) following SAT implementation (P<0.001), and the median door-to-IAT time also decreased from 156 min (IQR 124.5–212.5 min) to 86.5 min (IQR 67.5–102.3 min; P<0.001). As the onset-to-door time remained unchanged, the onset-to-IVT time (P=0.024) and onset-to-IAT time (P=0.002) also decreased. Such a reduction in the time for thrombolysis following SAT implementation was remarkable in the context of the recent 11-year trends at our hospital (Supplementary Table 2, Supplementary Figure 2).
The door-to-CT, door-to-MRI, and door-to-laboratory time did not differ between office hours and after-hours (P>0.05). Similarly, the door-to-IVT time was not different between office hours and after-hours (P=0.878). However, the door-to-IAT time was longer after-hours (P=0.020). Nevertheless, the door-to-IAT time after-hours following SAT implementation (median 100 min; IQR 78–154 min) was shorter than that during office hours before SAT implementation (median 135.5 min; IQR 103.8–183.5 min; P=0.058; Table 3).
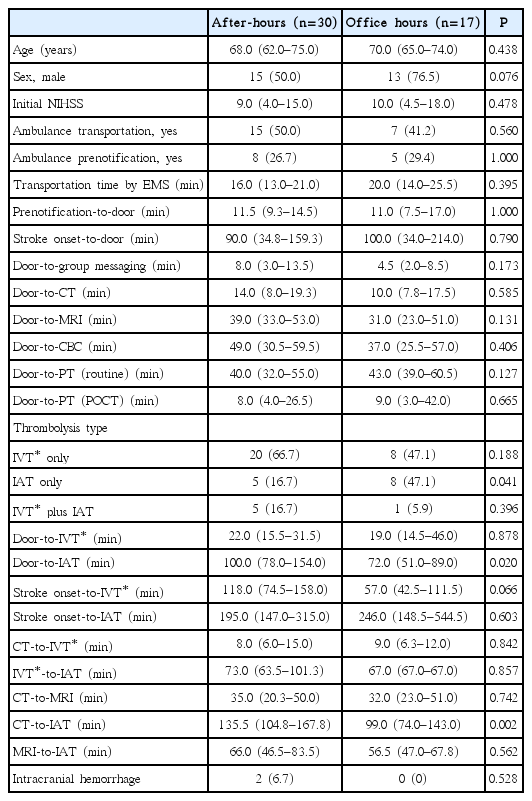
Baseline characteristics, time to evaluation, time to thrombolysis, and post-thrombolysis intracranial hemorrhage according to the time of hospital arrival following SAT implementation
For the 47 patients who visited the ER following SAT implementation, the door-to-IVT time in patients with ambulance prenotification (median 15 min; IQR 12–19 min) was shorter than that in patients without ambulance prenotification (median 26 min; IQR 20–36 min; P=0.001) (Supplementary Table 3). However, the door-to-IAT in patients with ambulance prenotification was not significantly shorter than that in patients without ambulance prenotification (P=0.473). For the 22 patients who visited the ER via EMS ambulance, the door-to-IVT time (P=0.008) and door-to-IAT time (P=0.044) was shorter for the 13 patients whose EMTs utilized prenotification than for the nine patients whose EMTs missed prenotification (Supplementary Figure 3).
Thrombolysis rate
A total of 198 patients received thrombolysis (IVT only: n=105; IAT only: n=57; IVT plus IAT: n=36) before SAT implementation, and 47 patients who received thrombolysis (IVT only: n=28; IAT only: n=13; IVT plus IAT: n=6) after SAT implementation. The total thrombolysis rate was 9.8% (198/2,012) before SAT implementation and 15.8% (47/297) after SAT implementation. The IVT rate was 7.0% (141/2,012) before SAT implementation and 11.4% (34/297) after SAT implementation. Therefore, the thrombolysis rate increased significantly following SAT implementation (total thrombolysis rate: P=0.002; IVT rate: P=0.007).
After SAT implementation, advance notification messages were sent to the neuroradiology intervention team in 18 cases, and IAT was performed for 15 patients due to confirmation of major vascular occlusion on magnetic resonance angiography. Advance notification group messages were not sent in 29 cases, but IAT was performed after multimodal MRI scans revealed vessel occlusions in only four of these cases (positive predictive value=83.3%; negative predictive value=86.2%).
Post-thrombolysis ICH
Out of 198 patients, 25 (12.6%) developed ICH before SAT implementation; of these, nine exhibited neurological deteriorations by four or more NIHSS scores (symptomatic ICH: 4.5%). Out of 47 patients, one (2.1%) developed ICH after SAT implementation, and none experienced neurological deterioration by four or more NIHSS scores (symptomatic ICH: 0%). The ICH rate was decreased after SAT implementation (P=0.035), and the symptomatic ICH rate was not different (P=0.213). The kappa coefficient of the interobserver agreement for ICH was 0.96.
Discussion
We implemented the SAT that was feasible for 24 h/day as a prospective performance improvement initiative to minimize the in-hospital delay for thrombolysis (i.e., IVT and IAT). Since SAT implementation, the median door-to-IVT time decreased from 46 min to 20.5 min, and the median door-to-IAT time decreased from 156 min to 86.5 min. We therefore achieved our pre-specified goals to decrease the time for thrombolysis. The total thrombolysis rate increased from 10% before SAT implementation to 16% after SAT implementation, and the IVT rate increased from 7% before SAT implementation to 11% after SAT implementation. The post-thrombolysis ICH rate decreased from 13% before SAT implementation to 2% after SAT implementation. Thus, SAT activities were potentially beneficial to patients experiencing an acute stroke.
Our prospective project commenced by reviewing the recent data and current status of thrombolysis in our hospital. Based on our recent data, we found that our key measures to be taken were to implement ambulance prenotification and reorganize the in-hospital process. Thus, we introduced ambulance prenotification, updated the thrombolysis protocol, specified time limits for each step, applied POCT, jettisoned unnecessary steps, administered tPA on the CT table, and sent group messages to SAT members for each step. These comprehensive activities and real-time peer reviews were feasible, did not require any changes to the overall hospital structure and manpower, and were effective for each step of the evaluation and management processes.
Our success in decreasing the time delay was likely not accomplished in only 4 months, and long-standing continued efforts to improve the hospital system underlie the current achievements. We previously demonstrated a significant reduction in the door-to-IVT time by changing our MRI screening system to CT-plus-MRI screening in December 2005, and by introducing a computerized physician order entry system for thrombolysis candidates in 2007 [10,13]. In addition, we relocated a new MRI machine beside the ER in 2010. Stroke center protocols were also updated every few years. Nevertheless, our current data showing a reduction in the door-to-thrombolysis time is remarkable in comparison with our previous efforts over the past decade.
The SAT was designed to be active 24 h/day, and no differences regarding the door-to-CT/MRI time, door-to-laboratory time, and door-to-IVT time were found between the office hours and after-hours after SAT implementation. However, the door-to-IAT time was longer after-hours than during office hours. Nevertheless, the door-to-IAT time after-hours following SAT implementation was shorter than that during the office hours prior to SAT implementation. Since other variables than the door-to-IAT time and CT-to-IAT time were delayed after-hours, we believe that the majority of these delays were due to the time required for the neuroradiologists to arrive at the hospital at night and on holidays. These findings suggest that interventions including the neuroradiologist’s early involvement in the assessment of thrombolysis candidates are also imperative as typically they do not remain at the hospital after-hours. For this purpose, advance notification provided to the intervention neuroradiologists may be helpful. Neurologist criteria for advance notification exhibited high positive (83%) and negative predictive values (86%) in the present study. However, further studies are required to identify proper methods to further decrease the door-to-IAT time, especially after-hours. Earlier initiation of IAT is associated with decreased mortality and morbidity [2,16]. However, no previous studies have reported efforts to decrease the door-to-IAT time. The median door-to-IAT time of 86.5 min in this study is real-world data and shorter than the times in any other recently published clinical trials [16-19]. We performed IAT in consecutive patients after-hours as well as during office hours.
Our study has some limitations that should be noted. First, the main outcomes of this study are the reduction in time to thrombolysis for the most recent 4-month period compared with the previous 28 months. A period of 4 months was sufficient to demonstrate improved temporal profiles, but not long enough to investigate clinical outcomes, such as the 3-month modified Rankin Scale. However, the therapeutic benefit of thrombolysis is the greatest when administered early after a stroke and declines over time. Lower rates of ICH after SAT implementation in this study may reduce patient morbidity and mortality. Our future studies will therefore investigate whether the SAT system can be maintained beyond several months and whether the saved time is related to better clinical outcomes. Second, because the hospital-initiated ambulance prenotification was not supported by the government or central EMS, we were required to contact each satellite EMS station and were only able to introduce prenotification in eight out of the 61 EMS stations. As a result, ambulance prenotification could only be utilized in <60% of the total EMS transportations. Simply using EMS to arrive at the hospital is not sufficient for thrombolysis; however, ambulance prenotification does enhance timely thrombolysis [20-22]. We showed that prenotification calls reduced the door-to-IVT time through reduction in door-to-CT time and door-to-POCT time. Therefore, government or a central EMS-initiated prenotification system is highly warranted. Third, imaging protocols could affect the time to thrombolysis, especially to IAT. We previously demonstrated that changing the imaging protocol from MRI to CT screening decreased the doorto-IVT time [10]. Similarly, the change in the imaging protocol from multimodal MRI screening into CT with CT angiography screening may additionally decrease the door-to-IAT time; further studies are required to address this issue. Fourth, although our SAT activities resulted in a significant reduction in the time for thrombolysis, this may not be directly applicable to other hospitals. In the Helsinki and Melbourne models, for instance, patients went straight to a CT room on ambulance stretchers, whereas we moved patients to the resuscitation room upon arrival and finished basic evaluations within 5 min. Five minutes was enough time to clear the CT room during the patients’ stay in the resuscitation room. Moving unstable patients directly to a CT table can be dangerous. We therefore believe that reorganization of the in-hospital process for thrombolysis should be done according to the specific situation of each hospital. Fifth, we performed POCT in most patients before infusion of tPA, which was followed by routine laboratory tests. However, POCT tests in the setting of thrombolytic therapies need to be validated in future studies.
Conclusions
Using a multidisciplinary approach, we showed that SAT significantly reduced in-hospital delay for thrombolysis treatment. SAT activity was also related to increased thrombolysis rate and decreased post-thrombolysis ICH. Time benefits of SAT were observed for both IVT and IAT, during both office hours and after-hours. Further studies to investigate whether reduction of inhospital delay is related to better clinical outcomes are needed.
Notes
The authors have no financial conflicts of interest.
Acknowledgements
We are grateful to EMTs, emergency physicians and nurses, neurology residents, radiology fellows, radiology technicians and nurses, laboratory technicians, security guards, office administrators, and neurological intensive care unit nurses.
Supplementary Material
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2016.01802.
Workflow for the Stroke Alert Team project.
Factors to enhance ambulance prenotification by EMTs
Trends in the total numbers and characteristics of stroke patients who visited the emergency room and those who received thrombolysis between March 2005 and August 2016
Baseline characteristics, time to evaluation, and time to thrombolysis according to the ambulance prenotification
The poster on the face arm speech time scale to educate emergency medical technicians. We created posters on the face arm speech time scale (FAST) scale to distribute to emergency medical technicians and local emergency medical service stations. These posters were posted on each ambulance and emergency medical service station. The Stroke Alert Team (SAT) phone numbers, hospital name, and hospital logo were not shown in the original version of this poster for local legal reasons.
In-hospital delay in administering thrombolysis. The 11-year trends of the median door-to-IVT time (A) and door-to-IAT time (B). Since SAT implementation (May 2, 2016), the median door-to-IVT time decreased to 20.5 min, and the median door-to-IAT time was also decreased to 86.5 min. SAT activities were prepared between January 1, 2016 and May 1, 2016, and implemented between May 2, 2016 and August 31, 2016. Error bars represent medians and 95% confidence intervals. IVT, intravenous thrombolysis; IAT, intra-arterial thrombectomy; SAT, the Stroke Alert Team. *With recombinant tissue plasminogen activator; †Between January 1, 2016 and May 1, 2016 (run-up period); ‡Between May 2, 2016 and August 31, 2016 (after SAT implementation).
Ambulance prenotification utilization in 22 thrombolysis patients who arrived at the hospital by EMS (A). The median door-to-IVT time and door-to-IAT time in 22 patients whose emergency medical technicians utilized ambulance prenotification (B and C). EMS, emergency medical service; IVT, intravenous thrombolysis; IAT, intra-arterial thrombectomy. *With recombinant tissue plasminogen activator.
