Intracranial Large Artery Disease of Non-Atherosclerotic Origin: Recent Progress and Clinical Implications
Article information
Abstract
Intracranial large artery disease (ILAD) is the major cause of stroke worldwide. With the application of recently introduced diagnostic techniques, the prevalence of non-atherosclerotic ILAD is expected to increase. Herein, we reviewed recent reports and summarized progress in the diagnosis and clinical impact of differentiation between ILAD of atherosclerotic and non-atherosclerotic origin. Our review of the literature suggests that more careful consideration of non-atherosclerotic causes and the application of appropriate diagnostic techniques in patients with ILAD may not only provide better results in the treatment of patients, but it may also lead to more successful clinical trials for the treatment of intracranial atherosclerosis.
Introduction
Intracranial large artery disease (ILAD) is the major cause of stroke worldwide. There have been significant advances in treatment strategies as a result of a better understanding of the pathophysiologic mechanisms of stroke underlying intracranial atherosclerosis [1-5]. Recently introduced diagnostic techniques, such as vessel wall imaging using high-resolution magnetic resonance imaging (HR-MRI) and genome-wide association studies (GWASs), enable us to differentiate intracranial atherosclerosis from ILAD of non-atherosclerotic origin. However, the prevalence of ILAD of non-atherosclerotic origin remains unclear. Although non-atherosclerotic ILAD is increasingly diagnosed, many patients with this disease may be misclassified as having intracranial atherosclerosis. We reviewed recent reports and summarized progress in the diagnosis and clinical impact of differentiating between ILAD of atherosclerotic and non-atherosclerotic origin.
Search strategy and selection criteria
We searched PubMed and ClinicalTrials.gov for articles published in English up to August 2017, using the search terms stroke, cerebrovascular disease, and intracranial stenosis. Additionally, we searched references from relevant articles and reviews. The final reference list was generated on the basis of originality and relevance to this topic. We did not discuss individual etiologies of non-atherosclerotic ILAD or imaging techniques in depth, since these topics are reviewed elsewhere [6-9].
Non-atherosclerotic ILAD
Intracranial arterial dissection
Cervicocephalic arterial dissection is a common cause of stroke in young adults and adolescents. Tearing of the vessel wall between the intima and media or adventitia may result in the formation of a thrombus within the lumen, leading to a critical occlusion of the vessel or a thromboembolic episode. Tearing can also cause intracranial bleeding. Intracranial dissection should be suspected in patients with a related clinical syndrome (e.g., sudden neck pain, connective tissue disease, or minor trauma), especially in those who are young and have no atherosclerotic risk factors, or show stenosis at sites of predilection (e.g., the middle cerebral artery segment adjacent to the sphenoid ridge, anterior cerebral artery adjacent to the falx cerebri, or intracranial vertebral artery [VA] near the origin of the posterior inferior cerebellar artery) [9-12].
Cervicocerebral artery dissection accounts for approximately 2% of all ischemic strokes but about 20% of strokes in the young and middle-aged [13]. The prevalence of intracranial dissection among those with ILAD remains unclear and it may be underestimated, since most large studies have examined carotid dissection in non-Asian countries where intracranial dissection is relatively rare, compared with the prevalence in Asia. In addition, spontaneous intracranial dissection may have been misclassified as intracranial atherosclerosis. Pain at the onset of stroke symptoms (a typical clinical feature of dissection), is not commonly reported in most clinical studies, and a history of trauma was more common in patients with extracranial dissection than in those with intracranial dissection [14]. Moreover, luminal imaging, including conventional angiography, may be insufficient for the diagnosis of intracranial dissection if patients do not show aneurysmal dilation.
In non-Asian populations, intracranial dissection is believed to comprise <10% of all spontaneous cervicocephalic artery dissections in adults [15]. However, intracranial dissection is more common than extracranial dissection in Asian populations, in both the anterior and posterior circulation [14,16,17]. Anatomical differences (i.e., intracranial vessel wall thickness and prevalence of arterial hypoplasia) among racial populations may account for the high prevalence of intracranial dissection in Asians. In addition, certain genetic differences may result in variation in the location of arterial diseases among ethnicities (e.g., genetic variation in the elastin gene and the location of the intracranial aneurysm) [18]. However, ethnic differences in the location of the arterial dissection should be interpreted with caution, since Asian studies tend to use more intracranial vascular imaging tests, including HR-MRI, that enable the detection of a greater number of cases of intracranial dissection.
Moyamoya disease
Moyamoya disease is an uncommon cerebrovascular disease that is characterized by progressive stenosis of the large intracranial arteries and a hazy network of basal collaterals. The main pathological changes in the stenotic segment in moyamoya disease include fibrocellular thickening of the intima, medial thinness, and a decrease in the outer diameter [19-22]. Regional differences in incidence and patient characteristics have been reported [23]. Moyamoya disease is more prevalent in East Asians than in Westerners. The population susceptible to moyamoya disease was estimated to be 16.16 million in East Asian countries [24]; however, the occurrence of moyamoya disease in Western countries has been increasingly reported [25].
It is often difficult to differentiate moyamoya disease from intracranial atherosclerosis in adult patients with ILAD. Unlike in childhood-onset moyamoya disease, distal internal carotid artery (ICA) involvement and moyamoya vessels may not be observed in the early phase of adult-onset moyamoya disease [26,27]. This suggests that the current criteria may have limitations for diagnosing adult-onset moyamoya disease. It was thought that moyamoya disease mostly occurs in children in Asia, and the hemorrhage rate is higher in adults than in children [28]. However, in contrast with previous reports, recent epidemiologic studies in Asians and Westerners revealed that patients with moyamoya disease are older (with peak age at 40s) and they have greater ischemia or are asymptomatic [25,29,30].
Others
Vascular inflammatory disease, vasospasm, and immunological disorders are also important causes of non-atherosclerotic ILAD [9]. Vascular involvement is attributed to either direct damage of the endothelium or smooth muscle by pathogenic processes (e.g., infectious disease or vasculitis) or indirect damage resulting from accelerated atherosclerosis and endothelial dysfunction (e.g., systemic lupus erythematosus or cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [CADASIL]) [9].
Careful history taking and appropriate laboratory testing are essential. Bacterial or fungal infections and tuberculosis should be suspected, especially in developing countries, endemic areas, and immunocompromised patients. In systemic vasculitis, central nervous system involvement typically occurs several years after the onset of systemic involvement. Primary angiitis of the central nervous system (PACNS) is a rare idiopathic vasculitis restricted to small leptomeningeal and parenchymal arteries and veins, without systemic involvement. Reversible vasoconstriction syndrome (RCVS) is a clinical and radiologic syndrome characterized by acute onset, severe and recurrent headache, and reversible vasoconstriction of the cerebral arteries [31]. Headache is the most common symptom in both RCVS and PACNS. The characteristics of headache are different between the two disorders: thunderclap headache, the main presenting symptom of RCVS, is rare in PACNS [32]. Although the presence of typical luminal features is necessary for the diagnosis of RCVS (e.g., multifocal segmental vasoconstriction that normalizes within weeks) and vasculitis (e.g., alternating areas of stenosis and dilation), the initial angiogram can appear normal in some patients [33-35]. Characteristic wall changes on HR-MRI could help to differentiate these two conditions [36].
Recent advances in the evaluation of ILAD
Vessel wall imaging
Luminal evaluation, such as catheter angiography, computed tomography angiography, and magnetic resonance angiography, is traditionally used to diagnose ILAD. Vessel wall imaging can depict the morphology of atherosclerotic plaques, arterial walls, and surrounding structures in the intracranial arteries, beyond simple luminal changes. In addition to intracranial atherosclerotic plaque, non-atherosclerotic pathological changes in the involved segment can be visualized with vessel wall imaging. For example, recent neuroimaging techniques, such as three-dimensional constructive interference in steady-state MRI and HR-MRI studies in patients with moyamoya disease, have demonstrated constrictive remodeling (e.g., narrowing of the arterial outer diameter) in affected segments, and concentric enhancement of the symptomatic segments, compatible with well-known pathological features of moyamoya disease [37-39]. A recent study conducted in the USA that included diverse ethnic groups, showed that vessel wall imaging using HR-MRI can significantly improve differentiation of the causes of ILAD when combined with luminal imaging [40]. In addition, the degree of enhancement on HR-MRI may be a marker for disease activity in non-atherosclerotic ILAD, including moyamoya disease and vasculitis [38,41,42]. At present, most studies use 3 Tesla (3T) MRI because it provides an image resolution sufficient to visualize structures inside the vessel wall. The recently introduced ultra-HR (7T) MRI has superior signal to noise and contrast-to-noise characteristics compared to 3T MRI, thereby providing a higher quality image [43-46]. This 7T MRI technique may even visualize vessel wall pathology in the absence of disease on conventional images. The imaging findings of intracranial plaques were validated with histopathology [43,47].
Catheter-based imaging
Intravascular ultrasound (IVUS) and optical coherence tomography (OCT, the light analog of IVUS) are intravascular imaging techniques used in interventional cardiology [48]. The results of several case reports suggest that these techniques may provide information for use in the selection of patients with intracranial atherosclerosis who may benefit from stent placement therapy [49]. These techniques could provide virtual histology to characterize the plaque in large intracranial vessels (distal ICA, VA, and basilar artery). An in vitro study using intracranial arterial segments with atherosclerotic plaques showed good correlation of virtual histology by IVUS and 7T MRI with histopathologic analysis [50]. However, these techniques require catheter angiography and were not studied in non-atherosclerotic ILAD.
Genetic and serologic biomarkers
Ongoing multinational GWASs will identify loci associated with specific stroke subtypes. However, GWASs in ischemic stroke are limited because of small sample sizes of patients with ILAD and of Asian populations where intracranial atherosclerosis is prevalent. A GWAS showed that certain genetic variants are associated with cervicocephalic dissection [51]. A brain-derived neurotropic factor gene polymorphism was reported to be associated with the severity of RCVS [52]. The presence of the ring finger protein 213 (RNF213) gene is associated with the greatest susceptibility to moyamoya disease in East Asians [53,54]. Several non-p.Arg4810Lys RNF213 variants were recently found in Caucasians and East and South Asian patients with moyamoya disease [54-57]. When trying to identify genetic polymorphism associated with intracranial atherosclerosis, it will be important to refine patient selection to avoid inclusion of non-atherosclerotic ILAD patients. Careful selection of intracranial atherosclerosis patients with the aforementioned neuroimaging techniques may be needed.
Several circulating blood biomarkers may be helpful in the identification of ILAD etiologies. For example, hyperhomocysteinemia and more recently, an elevated fibrillin-1 level (the release of an extracellular matrix glycoprotein by disruption of the medial layer), were reported in patients with cervicocephalic dissection [58-60]. On the contrary, caveolin-1 level was decreased in patients with moyamoya disease compared to those with intracranial atherosclerosis, suggesting that moyamoya disease is a caveolae (scaffolding proteins that are abundant in endothelial cells and are related to angiogenesis) disorder [61]. These protein levels may be related to the severity of vascular lesions [60]. Lastly, circulating genetic components, such as microRNAs, may play a role in the development of ILAD.
Clinical implications
Assessing the prevalence of atherosclerotic and non-atherosclerotic ILAD
The current classification systems for stroke subtyping are largely based on luminal changes in large cervicocephalic vessels and the presence of potential sources of cardioembolism. Documentation of the pathophysiologic mechanisms underlying ILAD determines the proportion of intracranial atherosclerosis and other etiologic subtypes. Recently, ILAD of non-atherosclerotic origin has been increasingly recognized, especially in Asian populations. As shown in Figure 1, prospective observational HR-MRI studies in various study populations including non-stroke subjects [62], young-age stroke patients [63], and acute stroke patients [64], showed that non-atherosclerotic ILAD is prevalent across a wide range of atherosclerotic risk factors. Misclassification of ILAD of non-atherosclerotic origin as intracranial atherosclerosis could partly account for the high reported prevalence of intracranial atherosclerosis in Asians.
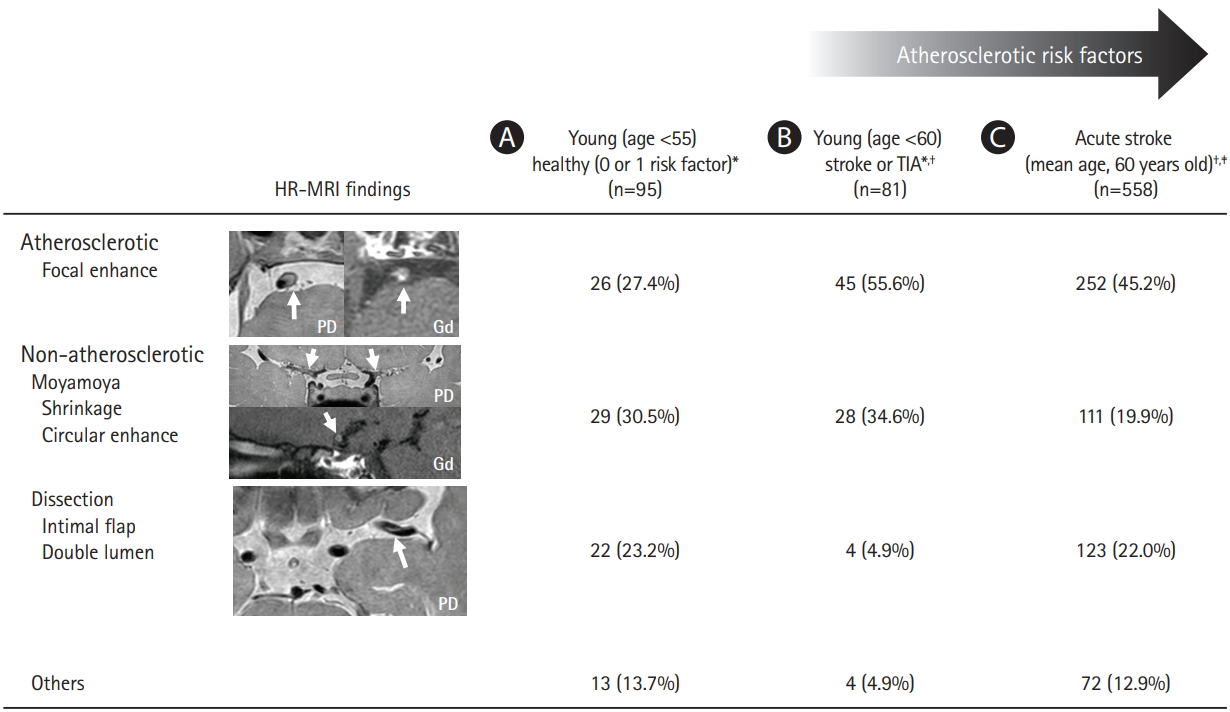
Prevalence of intracranial large artery disease of non-atherosclerotic origin demonstrated by high-resolution magnetic resonance imaging (HR-MRI) in (A) non-stroke subjects,[62] (B) young-age stroke patients,[63] and (C) acute stroke patients[64]. TIA, transient ischemic attack; PD, proton-density; Gd, gadolinium-enhancement. *Middle cerebral artery disease; † Excluding cases with typical luminal features of intracranial atherosclerosis (multiple tandem stenosis or carotid stenosis), moyamoya disease, or intracranial dissection; ‡ Both anterior and posterior circulation disease.
Intracranial dissection
Unlike carotid dissection, the pathognomonic luminal findings of arterial dissection, i.e., the presence of an intimal flap and double lumen, are rarely observed in small intracranial arteries (with a mean luminal diameter ~3 mm), even with conventional angiography. Imaging of intracranial vessel walls with HR-MRI generally uses a resolution of <1 mm and the definite diagnosis of intracranial dissection often requires HR-MRI. A HR-MRI study demonstrated that almost two-thirds of intracranial dissection cases were misclassified as intracranial atherosclerosis using current luminal imaging techniques [64].
Moyamoya disease
The annual incidence of moyamoya disease has reportedly increased in Japan, China, Taiwan, and Korea [65-68]. Such trends in the epidemiology of moyamoya disease may be accounted for by an increasing number of patients diagnosed with moyamoya disease rather than actual changes in the incidence of moyamoya disease. The recent interest in this disease could be the reason, as shown in Figure 2.
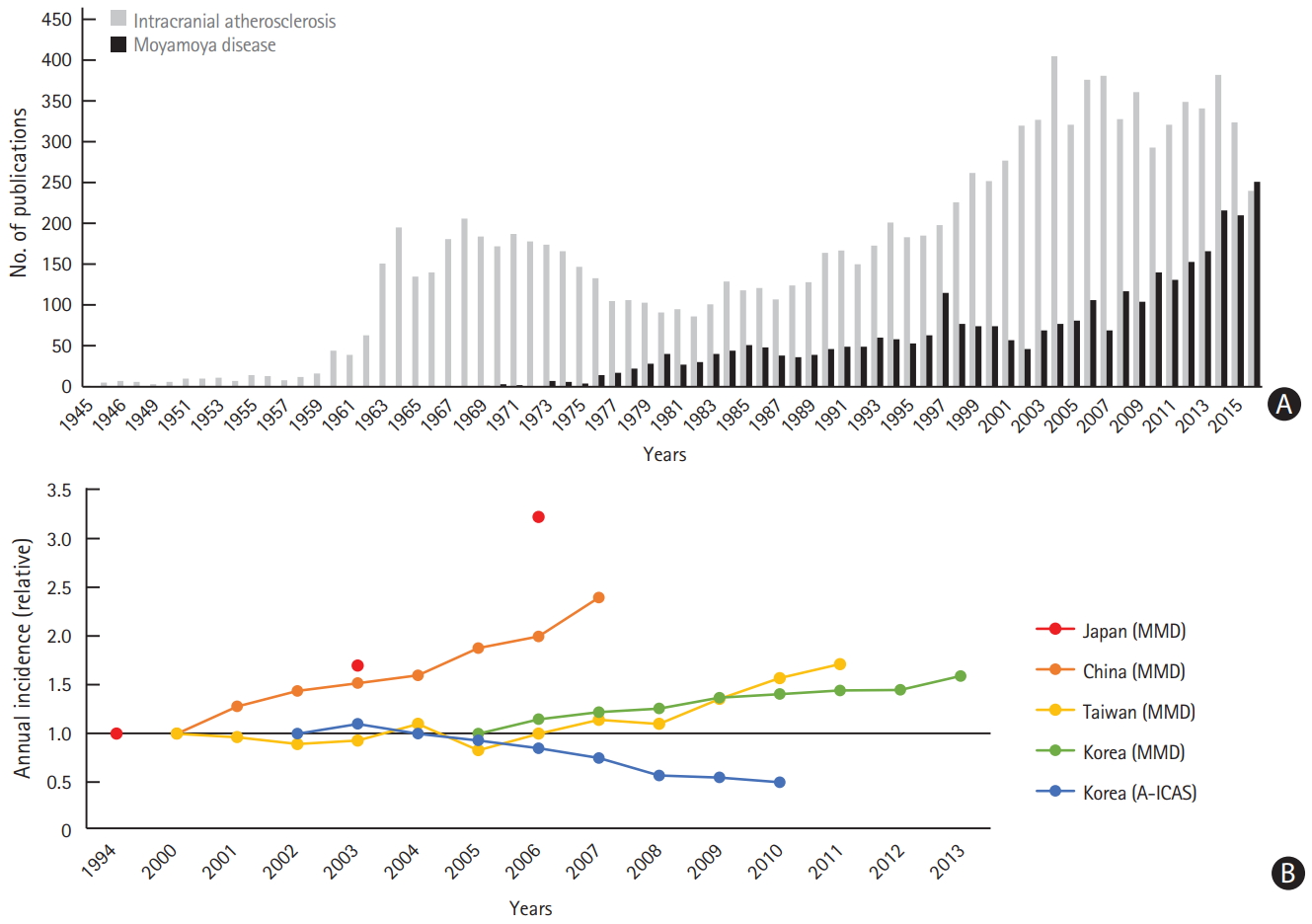
Trends of moyamoya disease (MMD) and intracranial atherosclerosis in Korea. (A) Increase in the number of publications on MMD and (B) increasing annual incidence of patients diagnosed with MMD in East Asian countries (nationwide data), with a decrease in the proportion of patients with anterior circulation intracranial atherosclerosis (A-ICAS) (nationwide hospital-based data)[65]-69.
Intracranial atherosclerosis
In contrast, nationwide, hospital-based data from Korea showed a decrease in the proportion of patients with intracranial atherosclerosis [69]. A recent pathologic study of 7,260 consecutive autopsy cases in Japan showed that the incidence and severity of intracranial atherosclerosis gradually decreased with later birth years over the last 50 years [70]. The authors suggest that this may be related to the development of therapeutic agents for the treatment of vascular risk factors and environmental changes.
Other causes
With the increasing use of serial vascular imaging and HR-MRI, the discovery of new disease entities and the number of involved patients are expected to increase in the future. For example, RCVS was first named in 2007 [31], and it has been increasingly recognized in recent years, although it is still an underdiagnosed disease entity [71].
Therapeutic perspective
Risk factor control, aggressive medical management (including statins), and stent placement (in selected patients) are important for preventing stroke in patients with intracranial atherosclerosis [2,72-74]. However, therapeutic strategies used in intracranial atherosclerosis may not be helpful or may even be harmful in some patients with non-atherosclerotic ILAD.
Intracranial dissection
The optimal treatment for patients with ischemic cerebrovascular disease due to intracranial dissection is unknown. The safety and effectiveness of thrombolysis or endovascular therapy for acute stroke and the choice of antithrombotic treatment (anticoagulants or antiplatelet agents) have not been assessed in randomized controlled trials [11,75]. Differentiation of intracranial dissection from intracranial atherosclerosis is important in young patients with ILAD, since the role of high-intensity statins in preventing stoke in intracranial dissection is unclear and unnecessary long-term use may cause complications.
Moyamoya disease
The pathophysiology of moyamoya disease is still unknown, and there is no evidence that pharmacological therapy can stop or reverse its progression [76]. Several case series consistently showed that the role of stenting in moyamoya disease is highly questionable and it is associated with a high rate of symptomatic restenosis/occlusion [77-79]. Revascularization surgery remains the mainstay of treatment for moyamoya disease, whereas recent guidelines do not recommend bypass surgery for intracranial atherosclerosis [80].
Other causes
Documentation of etiology is particularly important in ILAD associated with other causes. For example, immunosuppression is the mainstay of treatment in cases of vasculitis such as PACNS, but it has recently been reported that the use of steroids may contribute to worsening in patients with RCVS [81]. Use of HR-MRI enables RCVS to be differentiated from CNS vasculitis [82].
Research on intracranial atherosclerosis
Non-atherosclerotic ILAD misclassified as intracranial atherosclerosis has many clinical implications. First, it may lead to incorrect conclusions from clinical studies examining risk factors or biomarkers of intracranial atherosclerosis. A recent HR-MRI study showed that the risk factor profile of patients with misclassified intracranial atherosclerosis (no typical luminal changes of dissection, but HR-MRI showed dissection and no plaque) was similar to that of patients with frank intracranial dissection on luminal imaging, but different from that of patients with intracranial atherosclerosis [64]. These misclassified patients may obscure the risk factors characteristic of intracranial atherosclerosis. Second, misclassification could adversely affect the results of clinical trials for intracranial atherosclerosis (involving antithrombotic, statin, or stent management). It is interesting that in younger patients with anterior circulation (in particular, 88% of intracranial ICA lesions, who might have progressive vasculopathy of moyamoya disease), Wingspan stent placement had a high in-stent restenosis rate [83]. Third, the natural course and mechanisms of stroke in patients with ILAD differ among different pathophysiologies of ILAD. While spontaneous recanalization can be expected during follow-up in intracranial dissection, vascular stenosis progresses in patients with moyamoya disease. In addition, most patients with intracranial atherosclerosis have recurrent ischemic stroke, but hemorrhagic stroke is relatively common in most non-atherosclerotic ILAD cases, such as intracranial dissection, RCVS, and moyamoya disease.
Nevertheless, it should be noted that non-atherosclerotic ILAD may trigger intracranial atherosclerosis, and vice versa. First, genetic factors for non-atherosclerotic ILAD may influence the development of intracranial atherosclerosis. The RNF213 genetic variant associated with moyamoya disease was also observed in Japanese and Korean patients with nonmoyamoya ILAD [84,85]. These results may in part explain the high prevalence of intracranial atherosclerosis in Asians. Patients with this variant may be prone to atherosclerosis. The RNF213 variant could lead to vascular fragility, which may render vessels more vulnerable to hemodynamic stress and secondary insults [86]. Second, stiff, rupture-prone vessels in patients with underlying intracranial atherosclerosis are also susceptible to minor trauma, resulting in intracranial dissection in the elderly. Similarly, intracranial dissection could trigger atherosclerotic changes, and patients with intracranial dissection may be prone to premature atherosclerosis.
Conclusions and perspectives
With the application of new diagnostic techniques, the prevalence of non-atherosclerotic ILAD is expected to increase. Our review of the literature suggests that misclassification of nonatherosclerotic ILAD as intracranial atherosclerosis has clinical implications. More careful consideration of non-atherosclerotic causes and application of appropriate diagnostic techniques in patients with ILAD may not only provide better results in the treatment of patients, but it may also lead to more successful clinical trials for the treatment of intracranial atherosclerosis.
However, the application of new diagnostic techniques, such as HR-MRI, in ILAD patients has many limitations. First, HR-MRI sequences and techniques vary among studies. Optimal sequences and standardization to provide acceptable image quality and scanning time are needed. A collaborative international research network in China and North America (China-America MRI Plaque Imaging and Outcome Network [ChAMPION]) is ongoing. Second, routine application of the aforementioned diagnostic techniques is not possible in clinical practice. New diagnostic techniques may not be available, especially in low-income populations. Continuous efforts are needed to refine the approach to diagnosis of suspected non-atherosclerotic ILAD. For example, the use of HR-MRI could be considered in patients who are likely to have non-atherosclerotic ILAD, such as those with healthy risk factor profiles and no tandem stenotic lesions or calcification on luminal images. Lastly, in the area of extracranial large arteries such as carotid and coronary arteries, collecting arterial specimens from carotid endarterectomy provides a direct method to validate the capability of HR-MRI in identifying carotid plaque components. However, limited data on pathological correlation with in vivo MRI are available for ILAD, especially in non-atherosclerotic causes [87]. Further studies comparing MRI and histology are needed to validate the sensitivity and specificity of new diagnostic techniques in the differential diagnosis of ILAD. At the time of writing, we were aware of more than 10 active clinical trials on non-atherosclerotic ILAD (Supplementary Table 1). However, most trials involve a small number of patients and further studies with larger cohorts are warranted.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2018.00150.
Ongoing clinical trials of patients with intracranial large artery disease, excluding interventional/surgery trials
Notes
Disclosure
The authors have no financial conflicts of interest.
Acknowledgements
Drs. Masatoshi Koga and Hiroharu Kataoka (National Cerebral and Cardiovascular Center) provided useful advice.
This study was supported by grants of the Korea Health Technology R&D project (HC15C1056), the National Research Foundation of Korea (2018R1A2B2003489), an Intramural Research Fund for Cardiovascular Diseases of the National Cerebral and Cardiovascular Center, Japan (H28-4-1), and by a grant from the Ministry for Health, Welfare and Family Affairs, Korea (HI14C1985).