Association of Symptomatic Hearing Loss with Functional and Cognitive Recovery 1 Year after Intracerebral Hemorrhage
Article information
Dear Sir:
Survivors of intracerebral hemorrhage (ICH) are at high risk for poor functional and cognitive outcomes. At 12 months from the acute hemorrhage less than a third achieve functional independence, while over 25% are diagnosed with dementia and many more report milder cognitive deficits [1-3]. Hearing loss represents modifiable risk factor for functional decline cognitive dysfunction, yet it is often underdiagnosed and insufficiently addressed among individuals at risk [4]. We therefore sought to quantify the incidence of hearing loss among ICH survivors, identify associated risk factors, and determine whether it is associated with poor neurological recovery.
We analyzed data for consecutive patients admitted to Massachusetts General Hospital between January 1st 2006 and December 31st 2017 with a spontaneous ICH diagnosis [5]. Admission CT scans were analyzed to determine ICH location and hematoma volume [2]. We used validated ordinal scales to evaluate overall cerebral small vessel disease, cerebral amyloid angiopathy (CAA), and hypertensive arteriopathy burden on brain magnetic resonance imaging (MRI) scans obtained according to a previously validated protocol [1]. We initially screened for diagnosis of hearing loss by analyzing participants’ electronic health records (EHR) using a natural language processing approach [6]. All hearing loss diagnoses were then confirmed by manual review of EHR. We captured information on functional performance status on the modified Rankin Scale (mRS) at discharge, 3 months, and 12 months after ICH [7]. We then subdivided participants in the following groups: (1) functional decline (i.e., higher mRS at 12 months vs. 3 months); (2) functional stability (i.e., same mRS at 12 months vs. 3 months); and (3) functional recovery (i.e., lower mRS at 12 months vs. 3 months) [8]. We captured cognitive recovery by combining manual review of EHR with results from the modified Telephone Interview for Cognitive Status (TICS-m), administered at 3 and 12 months after ICH as previously described [2]. Among individuals with cognitive impairment at 3 months (major or minor neurocognitive disorder), we identified those who experienced cognitive recovery at 12 months based on either: (1) resolution of cognitive deficits (i.e., return to normal cognition) or (2) improvement from major to minor neurocognitive impairment. We performed univariable and multivariable analyses to identify risk factors for hearing loss diagnosis. We then performed multivariable analyses of likelihood to experience functional or cognitive recovery among study participants. For functional recovery, we created an ordinal logistic regression model quantifying likelihood of experiencing decline, stability, or improvement in functional performance. For cognitive recovery, we created a logistic regression model quantifying likelihood of experiencing improvement in cognitive performance (as previously defined). Additional information on study inclusion and exclusion criteria, enrollment procedures, data collection, and statistical methods are provided in the Supplementary Methods.
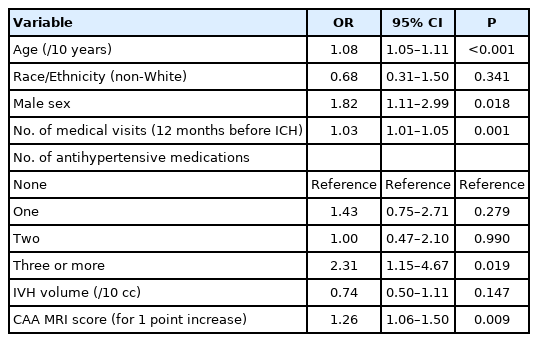
We initially screened a total of 1,339 consecutive ICH cases for inclusion in the present study. After application of exclusion and inclusion criteria (Supplementary Figure 1), we analyzed data for 737 ICH survivors. The majority of excluded participants (475/602, 78.9%) were excluded due to mortality within 1 year of the acute ICH. We identified 86 participants (11.7%) who received a diagnosis of hearing loss (Supplementary Table 1). In multivariable analyses, age, number of medical visits before ICH, number of anti-hypertensive medications used before ICH and CAA disease burden on MRI were independently associated with likelihood of receiving a diagnosis of hearing loss (Table 1). Among 737 participants, 60 (8.1%) experienced functional decline, 473 (64.2%) experienced functional stability, and 204 (27.7%) experienced functional recovery (Figure 1A). In multivariable analyses, hearing loss emerged as independently associated with functional recovery at 1 year from ICH (Table 2). At 3 months, 92 participants (12%) were diagnosed with minor neurocognitive disorder and 182 (25%) with major neurocognitive disorder, and were thus eligible for inclusion in subsequent analysis of cognitive recovery in the first year after ICH (Figure 1B). We found that 76/274 (28%) fulfilled criteria for cognitive recovery at 12 months from the initial hemorrhagic stroke event. In multivariable hearing loss was an independent risk factor for lower likelihood of cognitive recovery at 1 year from ICH (Table 2).

Functional and cognitive recovery following intracerebral hemorrhage (ICH) among survivors with and without hearing loss. (A) Comparison of distribution in modified Rankin Scale (mRS) scores at 3 months vs. 12 months among ICH survivors without (top bars) vs. with (bottom bars) hearing loss. Numbers in the bar section refer to count of individuals within each subgroup defined by mRS scores. (B) Comparison of distribution in cognitive status diagnoses at 3 months vs. 12 months among ICH survivors without (top bars) vs. with (bottom bars) hearing loss. Numbers in the bar section refer to count of individuals within each subgroup defined by diagnosis of major neurocognitive disorder (NCD), minor NCD, or normal cognition at each time point.
In summary, we leveraged data from a single-center study of ICH survivors to investigate the prevalence of hearing loss in this patient group at high risk for poor functional and cognitive outcomes. We found that over 10% of them displayed evidence of symptomatic hearing loss, with multiple factors contributing to individuals’ likelihood of receiving this diagnosis. We specifically identified a novel association with CAA disease severity, as quantified via a validated MRI scoring system. Furthermore, we found that hearing loss was associated with lower likelihood of good functional and cognitive outcomes at 1 year after ICH. Overall, our results indicate hearing loss might serve as a key, underappreciated barrier preventing survivors of primary ICH from achieving their maximum recovery potential. Additional studies will be required to investigate mechanisms accounting for this association, including determining: (1) impacts engagement with post-stroke rehabilitation effort; (2) serves as a surrogate marker of underlying brain health and its expected impact on recovery; and (3) directly contributes to decreased neuronal plasticity [9].
Our study has several limitations. Our approach likely resulted in imprecise capture of hearing performance—including potential for incorrect hearing loss diagnoses and limited ability to quantify etiology, laterality, severity, and treatment course of hearing impairment. We also utilized phone-based cognitive testing, which could potentially introduce bias towards worse cognitive performance among participants with hearing loss. To address this possibility, we conducted a validated screening of hearing performance prior to phone-based cognitive testing, as in prior studies [2]. We also conducted a parallel analysis using EHR-derived cognitive performance data to bolster our findings. Finally, we leveraged data from a single, tertiary care center with dedicated expertise in ICH management. This may have therefore introduced referral and severity bias, potentially limiting generalizability to ICH survivors at large.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2022.00836.
Participants’ characteristics
Flow chart of enrollment for study participants, indicating number of individuals initially considered for inclusion and removed based on specific exclusion criteria. ICH, intracerebral hemorrhage; CT, computed tomography; MRI, magnetic resonance imaging.
Acknowledgements
The authors’ work on this study was supported by funding from the US National Institute of Health (K23NS100816, R01NS093870, R01NS103924, and R01AG26484). The funding entities had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
All statistical analyses performed by Jessica R. Abramson, BA and Alessandro Biffi, MD (Massachusetts General Hospital).
Ms. Abramson and Dr. Biffi had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Notes
Disclosure
Ms. Abramson, Dr. Castello, Ms. Keins, Ms. Kourkoulis, Dr. Gurol and Dr. Viswanathan report no disclosures. Dr. Greenberg is supported by NIH R01AG26484. Dr. Christopher D. Anderson is supported by NIH R01NS103924, U01NS069763, the American Heart Association (AHA) (18SFRN34250007), the AHA-Bugher Foundation, receives sponsored research support from Massachusetts General Hospital and Bayer AG, and consulting for ApoPharma and Invitae. Dr. Rosand is supported by the AHA-Bugher Foundation, by NIH R01NS036695, UM1HG008895, R01NS093870, R24NS092983, and has consulted for Boehringer Ingelheim. Dr. Biffi is supported by Massachusetts General Hospital, the AHA-Bugher Foundation, and by NIH K23NS100816.