Smartphone App in Stroke Management: A Narrative Updated Review
Article information
Abstract
The spread of smartphones and mobile-Health (m-health) has progressively changed clinical practice, implementing access to medical knowledge and communication between doctors and patients. Dedicated software called Applications (or Apps), assists the practitioners in the various phases of clinical practice, from diagnosis to follow-up and therapy management. The impact of this technology is even more important in diseases such as stroke, which are characterized by a complex management that includes several moments: primary prevention, acute phase management, rehabilitation, and secondary prevention. This review aims to evaluate and summarize the available literature on Apps for the clinical management of stroke. We described their potential and weaknesses, discussing potential room for improvement. Medline databases were interrogated for studies concerning guideline-based decision support Apps for stroke management and other medical scenarios from 2007 (introduction of the first iPhone) until January 2022. We found 551 studies. Forty-three papers were included because they fitted the scope of the review. Based on their purpose, Apps were classified into three groups: primary prevention Apps, acute stroke management Apps, and post-acute stroke Apps. We described the aim of each App and, when available, the results of clinical studies. For acute stroke, several Apps have been designed with the primary purpose of helping communication and sharing of patients’ clinical data among healthcare providers. However, interactive systems Apps aiming to assist clinicians are still lacking, and this field should be developed because it may improve stroke patients’ management.
Introduction
The spread of digital health has profoundly changed clinical practice [1] in the last years, and the coronavirus disease 2019 (COVID-19) pandemic strengthened the use of such technologies [2,3]. Digital health represents the set of information and communication technologies that contribute to manage diseases and health risks, as well as promoting health and well-being [4]. Smartphones have accelerated the digitization process of medicine, leading to mobile-health (or m-Health), which has simplified both the communication between doctor and patient and the access to medical knowledge to improve patients management [5]. These new tools, using dedicated software called “Applications” (or Apps), assist the doctor in several phases of clinical practice, such as diagnosis, follow-up, and therapy management. Moreover, some Apps are designed as a clinical decision support system (CDSS). The function of these CDSS Apps is collecting and analysing clinical data in order to provide suggestions and reminders based on the latest guidelines. Thus, CDSS Apps improve the compliance with updated clinical recommendations [6]. A different kind of Apps, using video-assisted calls, allow remote clinical evaluations (telemedicine) [7], remote monitoring of vital parameters with the help of wearable devices (telemonitoring) [8] and management of clinical priorities even before patients arrival at the hospital (teletriage) [9]. In the United Kingdom, the proportion of phone or video medical visits rose from around 13% in late 2019 to 48% at the pandemic’s peak in April to June 2020 [10].
The impact of these technologies and the improvement allowed by these Apps becomes even more important in common and time-dependent diseases such as stroke. Stroke represents the second leading cause of death and the most significant cause of disability in the world, with an annual mortality of 5.5 million [11,12]. It represents 1.7% of healthcare costs in Europe with an annual cost of 60 billion EUR in Europe [13] and 45.5 billion USD in the USA [14]. Its impact on society is not only confined to acute management, but also rehabilitation, medical care of chronic management, social services, and informal caregiving have huge direct and indirect costs [15]. Several improvements have been proposed in recent years about stroke management, mainly for acute phase and specifically for reducing the time to provide treatment [16,17]. Every 15 minutes of delay in the administration of reperfusion therapies (thrombolysis and thrombectomy) leads to an increased risk of long-term disability, in-hospital mortality, and intraparenchymal hemorrhage [18]. Healthcare costs are also associated with the timing of reperfusion therapy and any delay is associated with a reduction in quality-adjusted life years and the economic value of care [19,20]. In this scenario, further improvement may be provided by implementation of Apps with the aim of speeding up patients’ management in acute stroke.
This review aims to assess and summarize the available literature on mobile phone Apps designed for the clinical management of stroke. We described their potential and weaknesses, discussing possible room for improvement.
Methods
We performed a comprehensive literature search review to identify all published studies relevant to stroke management smartphone Apps, searching MEDLINE (PubMed). Literature revision was performed independently by two researchers using pre-selected common keywords, and studies were chosen by consensus.
The string described in Table 1, was used in PubMed search engine for article selection. We included smartphone applications developed to support clinical decision-making in primary, pre-hospital, in-hospital, and chronic management in stroke. We included Apps for monitoring atrial fibrillation (AF) as a common risk factor for secondary ischemic stroke [21]. We have also included stroke-specific Apps for managing other risk factors: hypertension, diet, and diabetes. We included both clinically validated Apps and proof-of-concept studies.
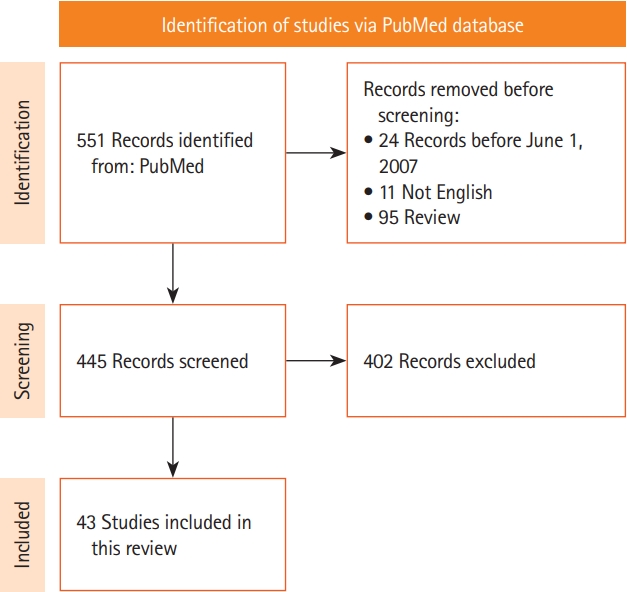
Considering that the first smartphone was released in 2007, we narrowed our search from June 1, 2007 to January 31, 2022. Exclusion criteria were: non-smartphone Apps and software, and non-stroke-specific Apps (calculators, messaging Apps, generic Apps for monitoring cardiovascular risk factors). The following data were collected: (1) study design; (2) functioning of the Apps; (3) reliability; and (4) efficacy in improving daily clinical practice. We arranged the Apps taking into account each step of stroke management: Primary prevention Apps, acute stroke management Apps (pre-hospitalization and in-hospital), and post-acute stroke Apps (rehabilitation and secondary prevention). The algorithm of paper selection is reported in Figure 1 and the search strategy in Table 1.
Results
We found 551 papers about stroke-related Apps. We then excluded duplicated articles or reports and publications different from research studies (e.g., reviews, letters, editorial, and commentaries), non-English papers, and any other study that did not fit with the aim of this review (Figure 1). We excluded applications not designed for smartphone (n=85), not stroke-specific Apps (n=168) mainly blood pressure sensing and management Apps (n=44), AF management Apps (n=95), bleeding risk management Apps (n=3), or obesity management Apps (n=7). After evaluation of the inclusion and exclusion criteria, 43 studies were included in this review (Table 2).
Primary prevention Apps
The Global Burden of Disease Study showed that 90.5% of stroke risk factors are modifiable [12]. Dietary changes (Mediterranean diet, low salt intake), physical activity, reduction of blood pressure levels, reduction of low-density lipoprotein and total cholesterol levels, and control of glycaemic levels in diabetic patients have been proven to reduce stroke events in individuals with high cardiovascular risk [21]. The Stroke Riskometer [22] App helps patients managing modifiable cardiovascular risk factors. Its algorithm was derived from the Framingham Stroke Risk Score (FSRS) prediction algorithm [23] and other additional major risk factors shown to be important for both ischemic and hemorrhagic strokes, largely based on the INTERSTROKE study [24]. It consists of items such as diet, familiarity for stroke, and physical activity. However, a parallel, 2-arm prospective, proof-of-concept randomized controlled trial failed to demonstrate a benefit of the Stroke Riskometer App compared with the standard of care in terms of cardiovascular risk reduction [25].
Acute stroke management Apps
Pre-hospital Apps
Stroke’s signs and symptoms non-recognition [26] and delayed ambulance transport [27] are major determinants of delayed door-to-needle time (DNT) for thrombolysis administration [28]. Apps can improve recognition of stroke signs even before emergency department admission. iLAMA [29], for example, is an augmented reality App that recognizes acute stroke symptoms thanks to the camera and the accelerometer of the smartphone. Indeed, iLAMA is able to evaluate eye motility, the presence of facial paresis, or the presence of dysmetria of the limbs through smartphone camera. Besides, the accelerometer allows to assess the presence of limb weakness. The data are then sent to a team of neurologists for analysis and the eventual activation of the emergency service [29]. Another App that aims to speed up stroke recognition is a smartphone-assisted pre-hospital medical information system (SPMIS), a platform for communicating stroke patient clinical data. Ambulances are equipped with a smartphone where the App is installed, ambulance crews will enter patient info and answer questions for pre-hospital diagnosis. The info is shared in real-time with the hospital medical staff even before the patient arrives to the emergency department [30].
The FAST-ED App [31], instead, represents the App version of the FAST-ED scale for large vessel occlusion (LVO) stroke diagnosis [32]. The smartphone application consists of a tool designed to assist Emergency Medical Service professionals in providing field assessment and destination triage of patients with acute ischemic stroke. It is based on a series of questions assessing patients’ conditions such as age, anticoagulant usage, last known healthy time, and symptoms to evaluate eligibility for intravenous recombinant tissue plasminogen activator (tPA) or endovascular treatment. It also has a database of all regional stroke centers according to their capability to provide endovascular treatment and Global Positioning System (GPS) technology with real-time traffic information to compute the transportation times to the different neighbouring stroke centers [31]. A retrospective study conducted on 2,815 patients affected by LVO showed that FAST-ED point ≥4 revealed very good accuracy in detecting LVO with an overall sensitivity of 77% and a specificity of 87% [33]. Similar to the FAST-ED App is the Egyptian Stroke Network (ESN) App [34], which features a screening tool based on questions aimed at detecting stroke signs, a video communication system to connect with the in-hospital stroke teams, and a real-time information system to localize the nearest hospital providing endovascular therapy. Outcomes such as DNT and vessel occlusion detection rate were evaluated by comparing ESN App and non-ESN App triage. Results show a reduction of the DNT (door-in-door-out time, 56±34 minutes vs. 96±45 minutes; door-to-groin puncture time, 50±7 minutes vs. 120±25 minutes; DNT, 55±12 minutes vs. 78±16 minutes with P<0.0001) and a higher rate of vessel occlusion detection using the ESN App [34].
Other Apps, such as Stroke119 [35], are developed for patients’ self-screening. The App includes a stroke screening tool based on the Cincinnati Prehospital Stroke Scale, real-time information on the nearest hospitals that provide thrombolytic treatment, and information on stroke symptoms and actions to take if an acute stroke is suspected [35].
In-hospital management Apps
Reduced adherence to guidelines [36], lack of communication between the ambulance team and hospital physicians [37] or among neurologists of first and second-level hospitals [38] seem to be the main factors of reperfusion therapies administration delay in the stroke intrahospital management. The implementation of communication and teleconsultation between consultants appears to be a key feature of Apps that assist intrahospital stroke management. For example, the JOIN App [39] allows to instantly share clinical and imaging data among stroke specialists involved in patient care. It consists of a chat, a DICOM viewer, and an encrypted two-way video system for video calls between practitioners. The app also consists of a milestones timestamp to record every step from home to hospital transportation to therapy onset [39]. A first study was conducted on 712 cases of acute stroke that were evaluated by neurology residents, followed via JOIN teleconsultation by a stroke neurologist. Another group was followed with a standard Picture Archiving and Communication System imaging workstation within 24 hours and analysed the decision made with remote assistance during the emergency setting. Results showed a significant reduction in DNT (63 with App vs. 90 minutes without App support) [40]. Another study evaluated the workflow of acute stroke management in the 2.7 years before JOIN implementation and in the 2.2 years after. Results show reduction in mean total time of treatment from 98.8 to 81.1 minutes, reduction in the mean times to initiation of tPA (from 81.0 to 64.3 minutes, P=0.003) and to the initiation of endovascular treatment (from 140.9 to 109.9 minutes, P=0.01) after JOIN implementation [41]. In another study conducted on 139 patient JOIN has shown to reduce DNT, door-to-puncture time (DPT), image-to-needle time (INT), and image-to-puncture time (IPT) compared with control group without App support (DNT, 62 minutes for the App group vs. 72 minutes for control group, P=0.038; INT, 42 minutes vs. 48 minutes, P=0.009; DPT, 106 minutes vs. 129 minutes, P=0.046; IPT, 89 minutes vs. 117 minutes, P=0.004) [42]. StopStroke [43] is another App that focuses on instant communication among physicians allowing real-time sharing of clinical data of stroke patients. Neurologists can enter patient personal and clinical info and chat or video-call the emergency team in order to streamline the acute stroke workflow. A retrospective analysis was conducted in 12 medical centers and the results showed a reduction of door-to-image time and DNT in patients treated with the help of the App compared to controls not assisted by the App.
Noone et al. [44] developed and studied the effectiveness of a mobile app-based strategy to reduce the DNT. The App, called Act-Fast, boasts a National Institutes of Health Stroke Scale (NIHSS) calculator, a thrombolysis checklist, and a toolbox to share images and notes among practitioners involved in the decision-making process. Results showed a considerable optimization of the stroke care pathway with a decrease in DNT of 16 minutes in the mobile App group versus the control group [44].
Compliance to guidelines and faster decision-making are essential for proper stroke management [36], since time is the main determinant of patient outcome [45]. Apps like Mayo clinic Acute Stroke Evaluation App [46] are developed like a digitized version of a workflow checklist for the management of acute stroke based on American Heart Association/American Stroke Association and NIHSS guidelines. The purpose of this App is to aid clinician with the decision-making process for thrombolytic therapy. A clinical study by Rubin et al. [46] evaluated guidelines adherence in the therapeutic choice of a group of residents aided by the App versus the therapeutic choice of the control group of residents not aided by the App. Results show that adherence to guidelines was higher in the App-assisted residents. A secondary endpoint was DNT, which was shown to be reduced by 16 minutes in the App-assisted group compared with the control group [46].
Post-acute stroke Apps
Rehabilitation Apps
As previously mentioned, stroke represents the leading cause of disability in the world [11,12]. Physical rehabilitation is a key part of post-acute management [47]. Studies have shown that starting rehabilitation in the first 2 weeks contributes to a reduction in long-term disability [48]. A Cochrane review reported the benefits of rehabilitation therapy in restoring function and mobility in upper limbs paresis following stroke, compared to patients not treated with rehabilitation therapy [49].
The use of the accelerometer and of the gyroscope embedded in the smartphone allows to collect data such as the type [50] and range of limbs movement [51-53], balance and posture [54] of stroke patients, either through smartphone or wearable devices such as smartwatches [53]. Some Apps also provide visual, audible and vibratory feedback in case of incorrect movements in order to assist and improve motor rehabilitation [52]. Other Apps use the features of virtual reality to improve the effectiveness of rehabilitation treatment [55-57]. Speed interactive pedalling training, for example, using smart phone-based motion-tracking technology has been shown to improve strength, balance, and gait in stroke patients [56]. Other Apps have CDSS functions: ViaTherapy allows a series of questions to assist in deciding the most appropriate rehabilitation workflow for a stroke patient [58]. Rehabilitation Guardian App [59] is characterized by four functional modules: health reminder, consultation, health information, and patient diary. The App gives medical information and provides rehabilitation exercises. Patients can enter their clinical information, exercises performed and questions about the rehabilitation process. The medical staff can access these modules, answer questions, and help with the management of the rehabilitation process remotely [59]. Regarding rehabilitation therapy, telemedicine demonstrates higher validity and reliability, as well as higher confidence and satisfaction perceived by patients, than the telephone assessment [60]. In addition, supervision of patients using exergames (video games with a rehabilitative function that promote movement aimed at improving strength and coordination of injured limbs) via teleconferencing could improve the effectiveness of exercise and limit errors [61].
Chronic management and secondary prevention Apps
A 2011 global meta-analysis estimated that 11% of stroke patients will have a 1-year recurrence of a second vascular event and 26% at 5 years [62]. Management of major risk factors for stroke recurrence such as hypertension, obesity, diabetes, and smoking, treated with antiplatelet/anticoagulant therapy, statins, and antihypertensive therapy may reduce the risk of secondary vascular events by 20% to 30% [63-66]. Many Apps aim to help patients manage their risk factors. The PRESTRO App [67] combines motivational support for a healthy lifestyle (physical activity, healthy nutrition, and smoking cessation), a reminder function for medication intake and blood pressure measurement and stroke education. Results from Fruhwirth et al. [67], clinical trial show that patients in the intervention group reported to be physically almost twice as active (13±9 hour/week) compared to controls (7±5 hour/week; P=0.022). More intense App usage was strongly associated with higher physical activity (r=0.60, P=0.005) and lower consumption of unhealthy food (r=−0.51, P=0.023). The Korea University Health Monitoring System for Stroke (KUHMS2) App [68] instead monitors parameters such as blood pressure, body weight, blood glucose, use of smoke/alcohol, and drug adherence. Results show a reduction in blood pressure level and HbA1c blood levels in patients who used the app compared to those who did not use it [68]. Lose it [69,70] is a weight loss App that has been evaluated in patients with minor stroke. The App works as an electronic food journal showing the values of the macronutrients of the foods consumed and a daily calorie count. Patients can save the meals consumed and the App gives reminders and weekly summaries [69]. The efficacy of an App for the management and promotion of Engaging everyday activities (EEA; i.e., daily activities that contribute to the reduction of risk factors for stroke) has been evaluated in subjects affected by transient ischemic attack showing promising results with an effective increase in EEA [71]. Movies4Stroke [72] is an App featuring a series of educational and informative videos for stroke patients. The videos contain useful advice on how to perform first aid, advice on activities with rehabilitative purpose, how to improve swallowing to reduce the risk of aspiration pneumonia, the drugs used in stroke and risk factors associated with a new stroke event [72].
Although AF is the leading cause of cardioembolic stroke, 9% to 25% of cases, the cause of embolism is not identified (embolic stroke of undetermined source [ESUS]) [73]. Detecting AF is critical to start anticoagulation therapy and reduce the risk of recurrent stroke, which is increased by approximately 2.1-fold in AF patients compared to AF patients on anticoagulation therapy.
Wearable devices can be used as detectors of AF. There have been several studies demonstrating that smartwatches can detect AF events [74]. Devices such as belts [75], miniaturized electrocardiograms (ECGs) associated with smartphone Apps [8,76], and devices that are placed on the patient’s chest have also been used [77,78].
Another useful App in the management of AF is AFib 2gether mobile App [79,80], which was developed by Pfizer Inc. (New York, NY, USA). It is a helpful tool for sharing decision-making regarding anticoagulation therapy for AF. Patients will enter their clinical data into the App, which will output the annual stroke risk score. Another App’s feature allows the patient to select a series of questions about anticoagulation therapy. The provider can review the data of the patient as well as any questions the patient solicited in the App for discussion prior to the visit. The aim of this App is to help the patient to do an informed decision about anticoagulation therapy [79,80].
Discussion
Patients with time-dependent diseases require several evaluations in a limited time-window, and stroke is a pivotal paradigm of this kind of diseases. Advanced tools, by implementation of the new technologies in clinical practice, capable of reducing evaluation, and treatment time, may be valuable both for patients and clinicians. In this narrative review, we summarized recent studies evaluating Apps used in stroke settings at each stage of management: pre-hospital stage, in-hospital stay, and rehabilitation period after discharge.
We found that the phase with the largest number of dedicated Apps is the rehabilitation phase. On the other hand, while intrahospital management of stroke has become more complex after the implementation of the extended windows of thrombolytic and endovascular treatment, making it difficult even for an experienced neurologist to make the right choice in the appropriate setting [45], there has been no simultaneous growth of Apps to assist the physician at this stage. Synthesizing the amount of information and complexity of newest treatment algorithms into an interactive CDSS system could simplify stroke patient management and improve adherence to guidelines. Among the Apps reviewed, only the Acute Stroke Evaluation App has shown to have similar features but, despite the good results of the study conducted, it is not currently available on the market. Other intrahospital applications focus on the creation of online teams to help in the management of the acute phase.
Each stage of stroke management has peculiar features, and these tools should face specific purposes. In the pre-hospital stage, diagnosis and reduction of DNT are the main determinants of patient outcome [45]. The final goal is to define more precisely symptoms onset timing, a fundamental parameter to set the right therapeutic pathway.
Some Apps have been developed to assist the recognition of symptoms (iLAMA [29]) and to smooth communication channels between rescuers and hospital. Other Apps like FAST-ED [31], SPSMS [30], ESN [34], and Stroke119 [35] allow to share patients’ data with the hospital neurologist, avoiding the loss of information during transport to hospital. On the other hand, adherence to guidelines represents one of the major determinant of patient prognosis in the intrahospital management of stroke [36]. Guiding practitioners in the right therapeutic choice is the main function of other available Apps. JOIN [39], Stop Stroke [43], and Act-fast [44] allow video calls with experienced neurologists to assist with the therapeutic decision. Mayo Clinic Acute stroke evaluation App [46] was designed with a CDSS framework and provides easy, instant access to guidelines but as previously mentioned the App was not updated with the new guidelines and extended windows of treatment.
After hospital stay, another important step in stroke recovery is neurorehabilitation. Speeding up the recovery, monitoring rehabilitation processes and controlling risk factors are the key features of the rehabilitation process in stroke. The spread of smartphone use had a massive impact in the rehabilitation phase of stroke as demonstrated by the large number of studies describing Apps specifically developed for improving this stage of stroke recovery. Moreover, the use of smartphone embedded sensors (gyroscope and accelerometer), along with additional wearable technologies, provides a constant monitoring of the rehabilitation phases quantifying and recording parameters such as walking, posture, and balance [50-54,81,82] and ensure continuous monitoring of vital parameters with the aim of a more comprehensive management of risk factors for stroke [74-78]. In addition, telemedicine-based technologies allow healthcare providers to remotely track patient’s exercise and progress [60]. Teleconsultation, however, is not always possible due to technological and logistical limitations such as the presence of an effective Internet network and the 24-hour presence of an active consultant. Regulation of the handling and sharing of sensitive data with third parties is another limitation to the use of this technology, as laws vary from one country to another. A stand-alone system that aids in faster and simplified consultation of new guidelines and recommendations is a possible goal for new applications.
Another important aspect in m-Health is the regulation and standardization of clinical software before the go-to-market [83]. This stage is reserved only for Apps that are configured as “software as a medical device,” whose intended use is for the diagnosis, cure, mitigation, or treatment of diseases [84]. Both U.S. Food and Drug Administration [84] and European union counterpart [85] distinguish between high health risk Apps (which need stricter regulation and require clinical validation through clinical trials) and low health risk Apps. In our review high-risk Apps are those with CDSS functionality such as FAST-ED and SPMIS that in response to patient data provide outputs characterized by therapeutic advice. Indeed, it is essential that the output returned by the App be controlled and standardized to avoid potentially risky therapeutic approaches. Other high-risk Apps are those implemented by sensors (such as rehabilitation and ECG analysis Apps). Clinical data collected from such Apps must be reliable and reproducible. In addition, any wearable devices must pass a technical validation that deems them safe for the patient [84,85]. Besides, the validation and regulatory phase is a step that can slow down software development and the go-to-market phase. Also, it could discourage any investment in field. On the other hand, scrutiny is required for software and devices used for medical purposes because they may pose a risk to patient health or privacy. Future legislation should focus on ways to streamline the review by regulatory agencies in order to reduce the waiting times while keeping adequate control procedures in place.
We were not able to find comparisons among studies in order to assess some potential strengths and weaknesses of available Apps because some of them were “proof of principle” studies, and trials were not available for all Apps.
Conclusions
Several studies evaluated the usefulness of Apps for improving management in the acute and chronic stages of stroke. For the acute phase of stroke, some Apps have been designed with the primary purpose of helping communication and sharing of patients’ clinical data among healthcare providers. However, interactive CDSS systems Apps aiming to assist clinicians are still lacking. More studies are warranted since such support tools may provide relevant advances for improving acute stroke management and clinical outcomes.
Notes
Disclosure
The authors have no financial conflicts of interest.
Acknowledgements
This work was supported and funded by the “Associazione Nazionale fra le imprese Assicuratrici” (ANIA).