Establishment of the Heart and Brain Team for Patent Foramen Ovale Closure in Stroke Patients: An Expert Opinion
Article information
Abstract
The online 2021 Asian-Pacific Heart and Brain Summit was organized to present and discuss experiences within leading Asian-Pacific centers with regard to institutional heart and brain teams managing the diagnosis, treatment, and follow-up of cryptogenic stroke (CS) patients with patent foramen ovale (PFO). This manuscript presents a narrative review of presentations and discussions during the summit meeting. Percutaneous PFO closure is an established therapy for CS patients in whom PFO is considered to be causal. Guidelines and consensus statements emphasize the importance of multidisciplinary clinical decision-making regarding PFO closure with the involvement of several clinical specialties, including neurology, cardiology, and hematology. It is also recommended that the patient be closely involved in this process. The heart and brain team is a collaborative platform that facilitates such a multidisciplinary decision-making process and patient involvement. It also creates opportunities for education and evaluation of the healthcare provided to patients with CS. This review provides insights into the implementation, composition, organization, and operation of a heart and brain team. Methods and metrics are suggested to evaluate the team’s role. We suggest that an efficient heart and brain team can implement guideline-recommended multidisciplinary clinical decision-making with regard to PFO closure in CS patients and play an important role in the management of these patients.
Introduction
Percutaneous closure of a patent foramen ovale (PFO) is an evidence-based treatment for preventing recurrent stroke in patients younger than 60 years of age who have a cryptogenic stroke (CS) with a high likelihood of being related to a PFO. Randomized controlled trials have demonstrated that PFO closure plus medical therapy achieves better stroke prevention in these patients than medical therapy alone [1-7]. Despite the strong results of these studies, the reduction in the risk of recurrent stroke differs across the CS population eligible for PFO closure, as shown by a patient-level meta-analysis of all six randomized PFO closure trials [8]. This illustrates the importance of an individualized approach, weighing all patient-specific benefits and risks based on the utilization of an extensive range of diagnostic methods in neurology and cardiology.
A heart and brain team is a multidisciplinary collaboration platform that facilitates an individualized decision-making process with equitable involvement of all relevant clinical specialties. In addition, this collaboration may promote ongoing education and knowledge building through the evaluation of clinical outcomes of patients managed by the team, irrespective of the eventual decision to perform or defer PFO closure.
This review aimed to provide insights into the composition and functioning of the heart and brain team to implement such a multidisciplinary approach to PFO closure in patients with CS. The review is based on presentations and discussions held during the online 2021 Asia-Pacific Heart and Brain Summit. During this meeting, several leading Asian-Pacific centers presented their experiences regarding patient selection, associated diagnostic pathways, treatment and follow-up of CS patients, and PFO closure, supported by a heart and brain team approach.
Why a heart and brain team?
While stroke and its direct consequences present within the brain, the heart often plays a crucial role in the etiology of stroke. This interrelatedness calls for a joint approach between neurology and cardiology. Such an approach may have a particular synergistic benefit if a cardiac intervention is considered as a potential treatment to prevent recurrent stroke, such as PFO closure in patients with PFO-associated stroke. Neurologists, and more specifically stroke neurologists, have expertise in neurological evaluation, neuroimaging interpretation, identification of stroke etiology, and management of stroke patients. Cardiologists and echocardiographers are experts in performing and interpreting cardiac imaging, assessing the PFO morphology, and detecting and managing cardiac arrhythmias. Interventional cardiologists have expertise in percutaneous catheter-based PFO closure techniques. Moreover, the involvement of the patient in the decision-making process may be facilitated by nursing staff members, who act as intermediaries between the team and the patient. Given the complex organization of modern healthcare, the formalization of this collaboration is desired to achieve effective synergy among all relevant specialties for optimal patient care.
Guidelines and consensus documents have emphasized the importance of the involvement of multiple clinical disciplines and the patient in decision-making regarding PFO closure [9-12]. The American Heart Association/American Stroke Association guideline on stroke management [11] states that “recommendations for PFO closure versus medical management should be made jointly by the patient, a cardiologist, and a neurologist.” In addition, approved intended use statements in the labeling of PFO occlusion devices [13,14] refer to joint decision-making by a neurologist and cardiologist. A heart and brain team embeds this collaboration in the healthcare organization as the primary institutional entity for diagnosis, clinical decision-making, and treatment of CS patients considered for PFO closure.
What does a heart and brain team do?
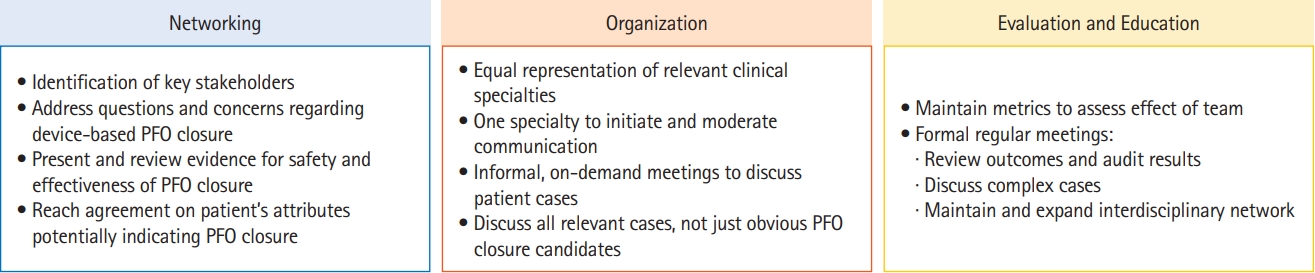
The heart and brain team is a multidisciplinary collaboration involving several clinical specialties who manage and coordinate various healthcare aspects regarding CS and PFO closure (Figure 1).
The heart and brain team as a multidisciplinary collaboration platform. PFO, patent foramen ovale; ECG, electrocardiogram; CT, computed tomography; MRI, magnetic resonance imaging; MR, magnetic resonance; TCD, transcranial Doppler; TEE, transesophageal echocardiography; RL, right-to-left; ASA, atrial septal aneurysm.
Typically, the neurology department is the main route through which patients with acute ischemic stroke symptoms enter the diagnostic pathway. The initial neurological evaluation is aimed at obtaining an image-based confirmation of the stroke, revealing its nature and location, and identifying the most likely stroke etiology. Diagnostic tests include short- and mid-term electrocardiogram (ECG) monitoring, use of cardiac imaging modalities including transthoracic echocardiography (TTE), carotid ultrasonography, transcranial Doppler ultrasound with bubble test (cTCD), lower limb Doppler ultrasound, and blood tests. Some tests may provide early direction for the diagnostic pathway. For example, the detection of deep venous thrombosis in combination with PFO revealed by TTE screening or the cTCD bubble test would direct the possibility of a paradoxical embolism. Conversely, early ECG screening may direct the diagnostic pathway towards a cardioembolic mechanism by the detection of atrial fibrillation (AF), a common cause of ischemic stroke. A comprehensive stroke workup is a prerequisite for the heart and brain team in the diagnosis and decision-making associated with the potential diagnosis of CS and consequent consideration of PFO closure.
If no known stroke etiology has been identified and paradoxical embolism is considered a potential cause, the patient is typically referred to the cardiology department for further investigation. At this point, the heart and brain team may get involved in facilitating multidisciplinary decision-making. Further cardiac imaging assessment mainly includes transesophageal echocardiography (TEE) to identify the presence of a PFO and to exclude other potential pathologies, such as atrial septal defect, valvular heart disease, or aortic arch atheroma. Most importantly, TEE provides crucial information about the PFO anatomy, the presence of high-risk PFO features such as an atrial septal aneurysm, a large right-to-left shunt with and without the Valsalva maneuver, and anatomical challenges to potential percutaneous PFO closure. If supported by the combined outcomes of all diagnostic assessments, the patient is diagnosed with CS with a likely causal role of the PFO, further evaluation within the heart and brain team is warranted.
As a first step in the decision-making process, the team evaluates the extent to which diagnostic outcomes support PFO closure. The evaluation should assess the completeness of neurological assessments to identify a known stroke etiology and exclude other cardioembolic mechanisms such as AF. Sufficient confidence should be achieved to exclude AF as a cardioembolic source of stroke. If needed, the team may recommend long-term cardiac rhythm monitoring and specific monitoring strategies to exclude AF, such as 30-day event monitoring or insertable cardiac monitoring (ICM). The Post-Embolic Rhythm Detection with Implantable vs External Monitoring (PER DIEM) trial showed superior AF detection with ICM monitoring compared to prolonged external monitoring [15]. However, the preferred monitoring strategy may depend on patient characteristics and risk factors that have been reported to be associated with AF detection by long-term monitoring, such as (among others) age, atrial enlargement, premature atrial beats, and a family history of AF [16-18].
The term PFO-associated stroke has been proposed as a distinct entity of ischemic stroke for all patients presenting with superficial, large deep, or retinal infarcts in the presence of a medium-to high-risk PFO and no other identified causes [19]. Once this diagnosis is established, the heart and brain team discusses and determines the preferred treatment. Again, this is a multidisciplinary discussion involving experts in neurology, cardiology, and interventional cardiology. The discussion focuses on the individual benefits and risks of potential treatment options, and is aimed at the development of an individualized treatment plan. For percutaneous catheter-based PFO closure, the PFO-Associated Stroke Causal Likelihood (PASCAL) classification system may be a helpful tool for estimating the expected treatment effect of PFO closure. This classification system predicts a more substantial benefit from percutaneous PFO closure with a higher risk of paradoxical embolism (RoPE) score [20] (≥7) combined with TEE findings of high-risk PFO features [8]. The specific risks to be evaluated include patient age, comorbidities, anatomical aspects, and specific patient conditions that may increase the procedural risk of PFO closure. Based on the assessed individual benefits and risks, the team discusses the preferred method of PFO closure (i.e., percutaneous vs. surgical), determines the optimal device for percutaneous closure, and makes recommendations regarding specific procedural aspects. Eventually, an individualized benefit-risk profile is developed to support the decision to close the PFO or pursue another strategy. As part of this strategy, antithrombotic therapy before and after the PFO closure procedure is discussed and decided upon.
Throughout the diagnosis and clinical decision-making process, the heart and brain team plays an important role in patient engagement and education. Consistent with the guidelines and consensus statements [9-11], clinical decision-making should involve the patient as a full participant in the process. Nursing staff members may support the involvement of the patient and also play a role in the coordination of diagnostic work-up and risk assessments, patient education, and providing guidance regarding lifestyle, medication, and diet. Patients eligible for PFO closure are relatively young compared to other stroke patients. These young patients are typically more concerned about stroke recurrence, post-stroke lifestyle impact, and bleeding risks associated with anticoagulation therapy than older patients. Given their younger age, they also prefer to make informed decisions through their own research. Patient education should address the benefits of PFO closure, such as reducing the risk of recurrent stroke and potential implications of stroke recurrence, as well as the associated risks, especially those related to the PFO closure procedure. The reimbursement aspect should also be addressed.
How to implement a heart and brain team?
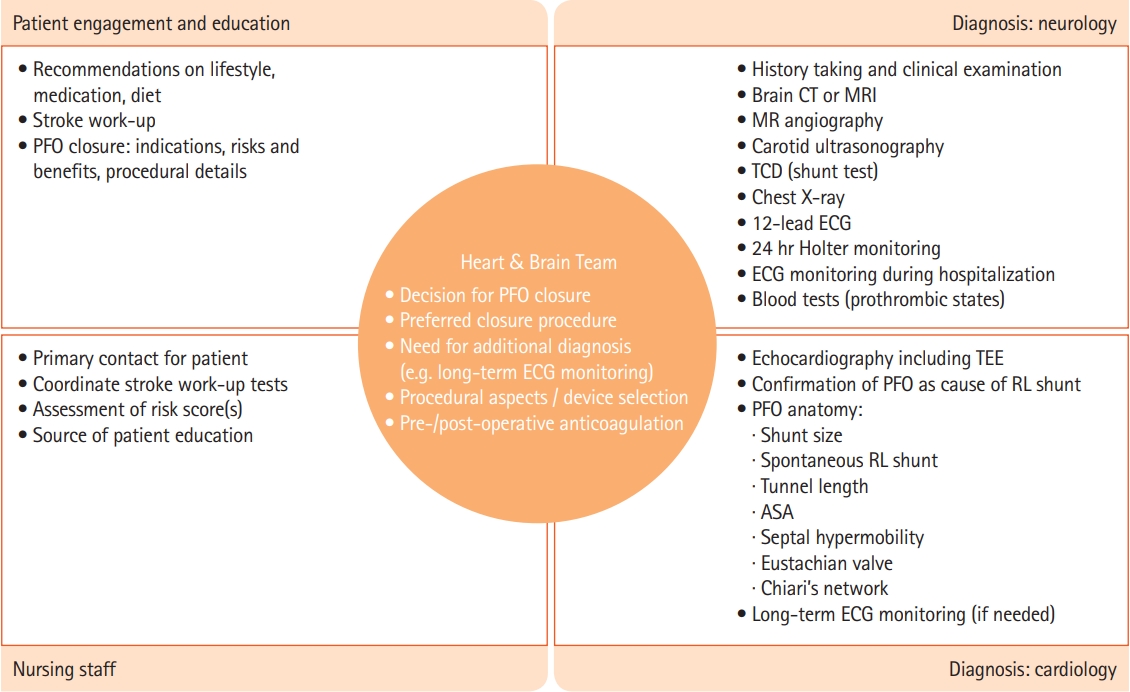
The actual implementation of a heart and brain team may follow a pragmatic approach adjusted to the local situation and organization of the clinical center in which the team should operate. Nevertheless, based on our experience, some best practices have been proposed (Figure 2).
The establishment of a heart and brain team requires extensive networking between relevant specialties, some of which may not consider PFO closure as an option for stroke prevention after CS. Awareness of the questions and concerns that may exist among key stakeholders is crucial for this networking process. The agreement that PFO is a biologically plausible route for paradoxical embolism is fundamentally important. Furthermore, concerns regarding procedural risks among clinicians not performing device-based therapies should be addressed within the context of clinical evidence for the safety of PFO closure procedures. Risks should be discussed against the background of the demonstrated benefits of PFO closure compared with medical therapy.
Although PFO closure is the main issue discussed by the heart and brain team, other issues may also be discussed, such as left atrial appendage occlusion (LAAO). Despite registry studies and clinical trials, the benefits of LAAO have not been properly established than that of PFO closure [21]. However, until more reliable trial results are obtained, LAAO may be considered in certain patients with AF-related stroke; for example, patients with recurrent strokes despite optimal medical management, those who have difficulties in taking oral anticoagulation/antiplatelets, or those who have issues of nonadherence [21,22].
The heart and brain team should consider developing a standard operating procedure to describe evidence-based decision-making within the team. Such a procedure should be tailored to the local organization (e.g., based on available diagnostic modalities) and should be regularly updated with new evidence and guideline revisions. Meetings of the heart and brain team may be held not only offline but also via a web-based video conferencing platform to facilitate broad attendance.
To establish and maintain an effective and committed heart and brain team, it is important that all relevant specialties are equally represented in the team and that discussions are not strongly restricted to only CS patients who are clearly eligible for PFO closure. In fact, the team may also discuss patients with other complex vascular problems, such as AF and a high degree of intracranial stenosis. Meetings of the heart and brain team to discuss individual patient cases may be informal and organized on an on-demand basis to facilitate timely decisions. One specialty, either neurology or cardiology, should initiate and moderate communication among all disciplines represented within the team. Neurologists capture inpatient information and manage referrals after the diagnosis. In addition to neurology and cardiology, other specialties may be involved on a case-by-case basis, depending on patient symptoms and specific diagnostic findings. A flexible organization of the heart and brain team around the neurology and cardiology core specialties ensures an expedited response time to the patient and minimizes patient waiting time and the risk of loss to follow-up. If allowed by the availability and organization of healthcare resources, a strict patient visit schedule may be utilized, allowing quick PFO closure within days of the index event. Obviously, such a strict time schedule is not feasible if a more time-consuming diagnosis, such as long-term cardiac rhythm monitoring, is required.
The use of metrics may be helpful in assessing effectiveness and supporting the added value of the heart and brain team. Primary metrics include the rate of recurrent stroke or transient ischemic attack (TIA), nature and incidence of periprocedural complications, residual right-to-left shunting, and bleeding complications among patients undergoing PFO closure versus those receiving other treatments. Additional aspects include the detection of other stroke etiologies after PFO closure, patients’ quality of life, and caregivers’ burden. All the findings should be formally reported and audited by the team.
In addition to informal meetings to discuss patient cases, the heart and brain team should schedule formal and regular meetings to exchange and evaluate experiences, review outcomes of patients managed by the team, and patient care-related metrics. Evaluations should include patient discussions within the team, irrespective of the decision to perform PFO closure or provide other treatments. Particular learning points may be obtained from the evaluation of complex cases and/or cases with limited direction from evidence-based guidelines. These meetings are excellent teaching opportunities and facilitate the bridging of different disciplines, help training fellows, expand the team, and promote collaboration.
Discussion
This review provides a shared view of the authors regarding the added value, implementation, and operation of a heart and brain team as a multidisciplinary collaboration platform for decision-making regarding PFO closure in CS patients. This collaboration has been proposed in the literature [23] and is supported by guidelines and consensus statements [9-12].
Despite the clinical evidence for PFO closure in CS patients, many questions remain unanswered [24]. First, most previous trials were conducted in young patients (<60 years), and the benefit of PFO closure in elderly patients remains unknown. Although the greatest added benefit of PFO closure plus medical therapy compared with medical therapy alone was found in patients with both a high RoPE score and a high-risk PFO (socalled probable PASCAL) [8], this observation may in part be attributed to the fact that older patients were excluded from the analysis. Actually, a low RoPE score (e.g., old age) alone was identified as an independent predictor of recurrent ischemic cerebrovascular events [25,26]. In a secondary analysis of the Device Closure Versus Medical Therapy for Cryptogenic Stroke Patients With High-Risk Patent Foramen Ovale (DEFENSE-PFO) trial that included older patients (≥60 years) [4], PFO closure was also effective in older patients, although the results were inconclusive due to the small number of events [27,28].
Second, PFO closure in stroke patients with other determined etiologies remains a matter of debate. A recent study suggested that PFO may be the actual cause of stroke in some patients with determined etiologies, especially in younger patients or those who belong to the probable PASCAL category [29]. Third, a possible benefit of PFO closure in patients with migraine with aura has been suggested, but remains unconfirmed [30]. Fourth, clinical decision-making is often complicated for patients with high-risk PFO and unsure diagnosis of TIA, and for CS patients with PFO who do not have ‘high-risk’ features. Finally, there is debate about the type and duration of antithrombotic therapy after PFO closure.
Only limited evidence-based guidance is available to address these questions, and extensive discussions within the heart and brain teams are needed to manage these controversial cases reasonably and appropriately. Such intense discussions may help us identify areas of future research with regard to PFO-associated stroke, which will eventually allow us to answer the questions listed above in the future.
Notes
Disclosure
Vincent Thijs: Dr. reports lecture fees and consultancy for Bayer, Boehringer Ingelheim, Pfizer/BMS, Medtronic, Abbott, and Biotronik; Kazunori Toyoda: Reports lecturer fees from Daiichi Sankyo, Bayer Yakuhin, Otsuka, Novartis, Abbott Medical, and Bristol-Myers Squibb, outside the submitted work; Bert Albers: Received an honorarium from Abbott for preparing this manuscript; Hans-Christoph Diener: Received honoraria in the last 3 years for contribution to advisory boards or oral presentations from Abbott, Actelion, BMS, Boehringer Ingelheim, Daiichi-Sankyo, Novo-Nordisk, Pfizer, and WebMD Global. Boehringer Ingelheim provided financial support for this research project.