Replacing Alteplase with Tenecteplase: Is the Time Ripe?
Article information
Abstract
Thrombolysis for acute ischemic stroke has predominantly been with alteplase for over a quarter of a century. In recent years, with trials showing evidence of higher rates of successful reperfusion, similar safety profile and efficacy of tenecteplase (TNK) as compared to alteplase, TNK has now emerged as another potential choice for thrombolysis in acute ischemic stroke. In this review, we will focus on these recent advances, aiming: (1) to provide a brief overview of thrombolysis in stroke; (2) to provide comparisons between alteplase and TNK for clinical, imaging, and safety outcomes; (3) to focus on key subgroups of interest to understand if there is an advantage of using TNK over alteplase or vice-versa, to review available evidence on role of TNK in intra-arterial thrombolysis, as bridging therapy and in mobile stroke units; and (4) to summarize what to expect in the near future from recently completed trials and propose areas for future research on this evolving topic. We present compelling data from several trials regarding the safety and efficacy of TNK in acute ischemic stroke along with completed yet unpublished trials that will help provide insight into these unanswered questions.
Introduction
The mainstay of acute ischemic stroke treatment is restoration of blood flow and improvement of perfusion to the affected region of the brain. Thrombolysis has been the standard of care for patients with ischemic stroke for over a quarter of a century, mainly dominated by alteplase. In recent years, with trials showing evidence of higher rates of successful reperfusion, similar safety profile and efficacy of tenecteplase (TNK) as compared to alteplase, TNK has now emerged as another potential choice for thrombolysis in acute ischemic stroke. In this review, we will focus on these recent advances. Our aims are: (1) to provide evidence for the use of TNK in acute ischemic stroke; (2) to provide comparisons between alteplase and TNK for clinical, imaging, and safety outcomes; (3) to focus on key subgroups of interest (wake-up stroke, extended time window, minor stroke, and posterior circulation stroke) and to review available evidence on role of TNK in intra-arterial (IA) thrombolysis, as bridging therapy and in mobile stroke units; and (4) to summarize what to expect in the near future from recently completed trials and propose areas for future research. The search strategy used for this review and historical overview of TNK use in ischemic stroke can be found in the Supplementary Material.
Evidence for use of tenecteplase in acute ischemic stroke
The initial stroke studies on TNK were focused on optimal dose finding and thus had safety as their primary outcome. TNK2SB (Phase 2B Study of Tenecteplase in Acute Ischemic Stroke) was one of the early studies within 3 hours of symptom onset using an adaptive sequential design. The high-dose TNK arm (0.4 mg/kg) was terminated early owing to higher rates of intracerebral hemorrhage (ICH). Overall, the study was terminated prematurely due to slow enrollment, and it could not demonstrate promise or futility for either the 0.1 mg/kg and 0.25 mg/kg TNK arms [1]. TEMPO-1 (Tenecteplase-Tissue-Type Plasminogen Activator Evaluation for Minor Ischemic Stroke with Proven Occlusion) compared 0.1 mg/kg TNK vs. 0.25 mg/kg in minor stroke (National Institutes of Health Stroke Scale [NIHSS] ≤5) and showed that patients in the 0.25 mg/kg TNK arm had higher recanalization rates, better functional outcomes with only one symptomatic intracerebral hemorrhage (SICH) out of 25 enrolled patients in this arm [2] Several subsequent trials have compared 0.25 mg/kg and 0.4 mg/kg TNK in different time windows with various efficacy-related primary outcomes. A detailed summary of the studies so far is provided in Table 1. Figure 1 gives an overview of the timeline for TNK use in medicine and details on the long history of TNK trials in cardiology and pharmacological properties of TNK compared to alteplase are provided in the Supplementary Material.

Timeline of the study and use of TNK in cardiology and ischemic stroke. TNK, tenecteplase; ASSENT-2, Assessment of the Safety and Efficacy of a New Thrombolytic Regimens 2; ACS, acute coronary syndrome; AIS, acute ischemic stroke; TNK2SB, Phase 2B Study of Tenecteplase in Acute Ischemic Stroke; ATTEST, Alteplase-Tenecteplase Trial Evaluation for Stroke Thrombolysis; NOR-TEST, Study of Tenecteplase Versus Alteplase for Thrombolysis in Acute Ischemic Stroke; EXTEND-IA TNK, Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke; AcT, Alteplase Compared to Tenecteplase in Patients With Acute Ischemic Stroke; NOR-TEST-2, The Norwegian Tenecteplase Stroke Trial 2; TWIST, Tenecteplase in Wake-up Ischemic Stroke Trial; TASTE-A, Tenecteplase Versus Alteplase for Stroke Thrombolysis Evaluation Trial in the Ambulance.
Comparison of tenecteplase with alteplase on various outcome measures
The trials to date have also provided us insights about various clinically relevant outcomes, besides the primary outcomes summarized in Table 1, including: (1) early neurological improvement (ENI), (2) 90-day disability outcomes, (3) surrogate imaging outcomes like successful reperfusion and early recanalization, and (4) safety outcomes like SICH and death. Our interpretation of the “weight” of the present evidence for these outcomes is summarized in Figures 2 and 3.

A visual representation of the current balance and quality of evidence from meta-analyses for key outcome measures of interest in comparing alteplase (r-tPA) to tenecteplase for thrombolysis in acute ischemic stroke. EVT, endovascular treatment; LVO, large vessel occlusion; LOE, level of evidence.
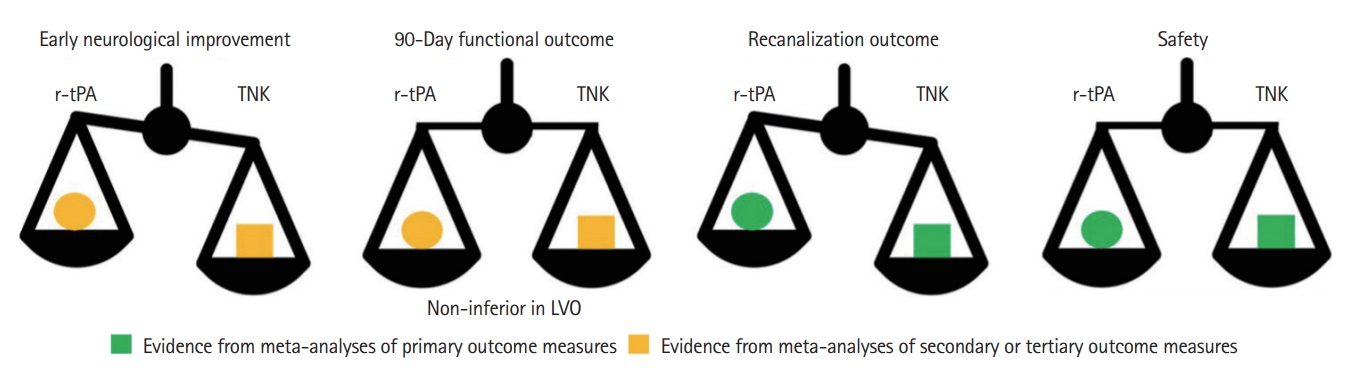
A visual representation of the current balance and quality of evidence from meta-analyses for key outcome measures of interest in comparing alteplase (r-tPA) to tenecteplase (TNK) for thrombolysis in acute ischemic stroke. LVO, large vessel occlusion.
Clinical outcomes
Early neurological improvement
ENI was not reported in all trials and the criteria differed across the studies, but they all involved substantial improvement in NIHSS by 24–72 hours. A pairwise network meta-analysis comparing alteplase and TNK including five randomized controlled trials (RCTs) (n=1,585) showed higher rates of ENI (odds ratio [OR] 1.43) in the TNK arm as compared to alteplase arm [3]. Another meta-analysis, which included only patients with large vessel occlusion (LVO) showed that the effect difference with TNK for ENI was 22 more per 1,000 as compared to alteplase [4].
90-Day disability outcomes
Within the randomized comparisons, NOR-TEST (Study of Tenecteplase Versus Alteplase for Thrombolysis in Acute Ischemic Stroke) was the largest trial (n=1,100) which tested for superiority of TNK, albeit high dose (0.4 mg/kg) over alteplase. The overall study did not show any differences in 3-month modified Rankin Scale (mRS) but was criticized for including a high number of mimics (16.6%) and patients with mild strokes (median baseline NIHSS 4) [5]. A meta-analysis including patients with LVO alone showed that patients with confirmed LVO receiving TNK had higher odds of mRS 0–2 (OR 2.06, 95% confidence interval [CI] 1.73–5.40) [4]. A formal non-inferiority (NI) meta-analysis of the five RCTs (TNK2SB, Australian TNK study, ATTEST [Alteplase-Tenecteplase Trial Evaluation for Stroke Thrombolysis], NOR-TEST, and EXTENDIA TNK [Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke]) with primary outcome of mRS 0-1 (free from disability) using different NI margins (6.5% as per NI design of the ENCHANTED (Enhanced Control of Hypertension and Thrombolysis Stroke Study) trial [6], and stricter NI margins of 5% and 1.3% based on stroke surveys among experts) for the lead statistical analysis. The unadjusted cumulative rates of mRS 0–1 were 57.9% with TNK and 55.4% with alteplase. The lower 95% CI bound of -4% fell within the lead -6.5% and intermediate -5% NI margins, but not within the most stringent -1.3% margin [7]. The AcT (Alteplase Compared to Tenecteplase in Patients With Acute Ischemic Stroke) trial [8], a pan-Canadian multicenter pragmatic registry linked trial, showed that TNK (0.25 mg/kg) is non-inferior to alteplase (0.9 mg/kg) (unadjusted risk difference 2.1% [95% CI -2.6 to 6.9]) with one-sided NI margin of 5% when given to patients with acute ischemic stroke in routine clinical practice. The trial included 1,600 individuals and showed that TNK is non-inferior to alteplase in acute ischemic stroke treated within 4.5 hours from symptom onset. 9 The results of this trial suggest TNK to be a reasonable alternative to alteplase in the <4.5 hours time window [10]. On the other hand, NOR-TEST-2 (The Norwegian Tenecteplase Stroke Trial 2) part A trial aimed to test whether higher dose of TNK (0.4 mg/kg) is non-inferior to alteplase in moderate or severe stroke. After having included 216 patients, the trial was terminated prematurely due to an increased number of SICH and mortality in the TNK (0.4 mg/kg) group: 6% vs. 1% and 15.6% vs. 4.8%, respectively [11]. The proportion with a favorable outcome (mRS 0–1) at 90 days was lower in the TNK group (32.3% vs. 51.5%). Thus, 0.4 mg/kg dose of TNK yielded worse safety and functional outcomes than alteplase in moderate or severe stroke [12]. The results of this study emphasize the need to use standard dose (0.25 mg/kg) of TNK, mainly due to safety concerns with higher dose (0.4 mg/kg).
Surrogate imaging outcomes: successful reperfusion and early recanalization rates
In a pooled analysis of the Australian TNK study and ATTEST study (n=146), 69 patients had a thrombolysis in cerebral infarction scale (TICI) 0/1 at baseline. The study showed that TNK-treated patients had greater complete recanalization rates (defined as TICI >2b/3 on follow-up CT angiography/MR angiography) as compared to alteplase (71% vs. 43%, P<0.001) [13]. EXTEND-IA TNK part 1 was designed to test early reperfusion of occluded arteries in patients receiving 0.25 mg/kg TNK versus alteplase within the 4.5-hour window. Substantial reperfusion was defined as reperfusion of >50% or absence of retrievable thrombus. The median interval from start of intravenous thrombolysis (IVT) to first digital subtraction angiography run was 54–56 minutes and the study found significantly higher rates of successful reperfusion in the TNK arm as compared to the alteplase arm (22% vs. 10%, P=0.0002 for NI and P=0.03 for superiority) [14]. For the remaining RCTs, successful reperfusion was a secondary outcome measure. In a meta-analysis of patients with LVO, patients with confirmed LVO receiving TNK had higher odds of successful recanalization (OR 3.05 [95% CI 1.73–5.40]) [4]. All these studies show that TNK has significantly higher rates of recanalization as compared to alteplase; however, robust data on whether this translates into better clinical outcomes is still lacking.
Safety outcomes
The meta-analysis by Burgos and Saver [7] and the AcT trial [8] showed that the unadjusted SICH rates were similar in both TNK and alteplase arms (meta-analysis: 3%, risk difference 0% [95% CI -1% to 2%]; AcT trial: 3.4% in TNK arm and 3.2% in alteplase). Mortality rates in the meta-analysis were slightly lower in the TNK arm (7.6%) versus alteplase arm (8.1%) but were similar in the AcT trial (15.3% in TNK arm and 15.4% in alteplase arm) [8]. Though point estimates were favorable, CIs for TNK crossed the narrow NI margins set for both SICH and mortality [7]. Other safety outcomes like any bleeding and angioedema were not reported in all trials, but there were no apparent differences between the groups. EXTEND-IA TNK part 2, which compared 0.25 mg/kg TNK with 0.4 mg/kg of TNK showed higher rates of SICH with higher dose (4.7% vs. 1.3%) although this was not statistically significant [15].
Key subgroups of interest
Precision medicine is getting more relevant in stroke care. Thus, in a future world where both alteplase and TNK are routinely available for use, we may need to identify certain situations wherein use of alteplase is more advantageous over TNK and vice versa. The current quality of evidence regarding the use of TNK in some of these relevant subgroups is illustrated in Figure 2, and we will discuss the evidence for each of these groups below.
Wake-up stroke and extended time window
The WAKE-UP (Efficacy and Safety of MRI-Based Thrombolysis in Wake-Up Stroke) trial which randomized patients with wake-up stroke and unknown onset into alteplase and placebo based on diffusion-weighted imaging (DWI)–fluid-attenuated inversion recovery (FLAIR) mismatch showed that patients who received alteplase had significantly better outcomes as compared to those who did not receive thrombolysis [16]. Such data is limited with TNK; however, the NOR-TEST trial included patients with wake-up stroke based on DWI-FLAIR mismatch (n=45). After excluding mimics in this population (n=5), there was no difference in excellent functional outcomes between the TNK and alteplase groups. Patients treated with TNK showed significantly better rates of ENI as compared to alteplase (87.4% vs. 54.2%, P=0.027). No ICH was detected on follow up scan in either arm [17]. To evaluate TNK in the extended time window, the TEMPO-1 study compared 0.1 mg/kg versus 0.25 mg/kg for patients with minor stroke (NIHSS ≤5) up to 12 hours from symptom onset (n=50). The study showed patients in the 0.25 mg/kg TNK arm had higher recanalization rates, better functional outcomes, and only one SICH [2]. TEMPO-2 (A Randomized Controlled Trial of TNK-tPA Versus Standard of Care for Minor Ischemic Stroke With Proven Occlusion; NCT02398656) is a similar ongoing phase 3 trial, randomizing patients who present with minor stroke (NIHSS ≤5) with either vessel occlusion or perfusion deficit into receiving either 0.25 mg/kg TNK or standard care (antiplatelets). The study has finished 650 of the planned 1,077 enrollments. The results of the TWIST (Tenecteplase in Wake-up Ischemic Stroke trial) [18] was presented recently at an international stroke conference but are yet unpublished; the study aimed to investigate if TNK (0.25 mg/kg) compared to no thrombolytic treatment in wake-up stroke patients (within 4.5 hours of wake-up) selected by non-contrast CT imaging results in better functional outcome measured by the mRS score (using ordinal shift analysis). The original plan was to include 600 patients and the final inclusion stopped at 578 patients. Of these, 288 (56.9% men) were randomized to receive TNK and 290 (57.9% men) in the control group. Baseline NIHSS was similar in both groups (median 6), however, thrombectomy was more common in the control group than in the TNK group (14.5% vs. 6.3%). The TNK arm had numerically better outcomes but it was not statistically significant on shift analysis of mRS (adjusted OR 1.18 [95% CI 0.88–1.57, P=0.27) or for 90-day mRS 0–1 (45% in TNK vs. 38% in control, adjusted OR 1.33 [95% CI 0.94–1.87 P=0.10). However, the study was limited by its small sample size and the higher rates of endovascular treatment (EVT) in the control arm may have mitigated the effect of TNK in the study arm [19]. TIMELESS (Tenecteplase in Stroke Patients Between 4.5 and 24 Hours; NCT03785678) is an ongoing placebo-controlled RCT using TNK 0.25 mg/kg for patients in the extended time window defined by the DEFUSE-3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3; NCT02586415) criteria, who may or may not be eligible for EVT. The results of these studies will provide further guidance on the use of TNK in the extended time window and for patients with unknown onset time. ETERNAL (Extending the Time Window for Tenecteplase by Effective Reperfusion in Patients with LVO; NCT04454788) is testing TNK 0.25 mg/kg as compared to alteplase 0.9 mg/kg in patients with LVO stroke in anterior circulation with target mismatch on CT perfusion. POST-ETERNAL (Extending the Time Window for Tenecteplase by Recanalization of Basilar Artery Occlusion in Posterior Circulation Stroke; NCT05105633) will be testing the same question as above in patients with basilar artery occlusion (BAO) and is yet to start recruitment. Thus, the future holds promise and we may know more about use of TNK in the extended time window and unknown onset trials with a direct comparison to alteplase.
Minor stroke
A subgroup analyses from the NOR-TEST trial, one including patients with minor stroke in the 3–4.5 hours window, showed that in a population with median NIHSS of 3, patients receiving TNK had higher odds of achieving good functional outcome as compared to alteplase (OR 1.19, 95% CI 0.68–2.10). The rates of SICH and mortality were similar in both groups [20]. It is worth noting that the trial used a relatively higher dose of TNK (0.4 mg/kg). TEMPO-2 trial (mentioned above) is also testing TNK in patients with minor non-disabling stroke in extended time window.
Elderly population
Octogenarians have greater frailty with poor baseline status due to presence of multiple comorbidities and have associated premorbid disability. An individual patient data meta-analysis from RCTs comparing alteplase versus placebo in this subgroup showed that elderly patients who receive alteplase have a higher proportion of good stroke outcomes, although they are two times more likely to have fatal ICH [21]. Thus, safety is of critical importance in this subgroup. A pooled analysis of EXTEND-IA TNK trials including patients over 80 years (n=137) showed that TNK was associated with improved 90-day mRS and reduced mortality rates in patients who received 0.25 mg/kg TNK versus 0.4 mg/kg TNK as well as in those who received 0.25 mg/kg TNK versus alteplase. None of the patients treated with 0.25 mg/kg TNK developed SICH [22]. A subgroup analysis of elderly patients (≥80 years) from the NOR-TEST trial (n=273) showed a numerically higher proportion of patients with excellent functional outcomes (mRS 0–1) after receiving TNK, but this was not significant even after excluding stroke mimics. The frequency of SICH and mortality was similar in the two groups (8.5% vs. 7% and 14.3% vs. 15.3%, respectively) [2].
Posterior circulation stroke
There is little but encouraging evidence to support the use of TNK in posterior circulation stroke, mainly BAO. A recent Australian retrospective analysis of pooled data from the BATMAN registry (clinical and procedural data of consecutive patients with BAO from the Basilar Artery Treatment and Management) and EXTEND-IA TNK trial, which included 110 patients with BAO treated with IVT prior to EVT showed that TNK (0.40 mg/kg or 0.25 mg/kg) was associated with higher rates of reperfusion as compared to alteplase (risk ratio 4.0, 95% CI 1.3–12, P=0.02), and there was no difference in SICH between the two groups (0 in the TNK arm vs. 1 in alteplase arm). Functional outcomes were similar in both groups, but the study was overall underpowered to detect these differences [23].
Intra-arterial thrombolysis
Currently, IA thrombolysis is used in selected patients who undergo EVT but have a distal target occlusion which are not amenable to mechanical thrombus retrieval. Alteplase is the routinely used thrombolytic for this purpose, and the recently published CHOICE (Intraarterial Alteplase Versus Placebo After Mechanical Thrombectomy) trial that tested adjunct use of IA alteplase compared to placebo showed a greater likelihood of excellent functional outcome in the alteplase arm [24]. The use of IA TNK for this purpose has yet to be tested in a large clinical trial. A recent small study retrospectively compared 33 patients IA TNK (1.5–10 mg) and 48 patients with alteplase (max dose 22 mg). The study found that patients treated with IA TNK had non-significant trend towards favorable clinical outcome at 1-month (OR 2.8, 95% CI 0.96–8.1, P=0.06) and there was no difference in hemorrhage rates comparing groups [25].
Bridging therapy
Currently, there is equipoise in the stroke community around the added benefit of thrombolysis in patients who present with acute LVO stroke eligible for EVT. Multiple RCTs conducted in the recent past have shown variable results. However, all these studies have tested the utility of thrombolysis with alteplase only in patients who present to a comprehensive stroke center (CSC). A French retrospective study assessed early recanalization rates on repeat imaging, in transfer patients alone receiving either alteplase or TNK using propensity score matching. The study included 131 matched patients in each arm and found that early recanalization rates were higher in TNK as compared to alteplase (21.4% vs. 18.3%) but this was not statistically significant [26]. Another large retrospective study of 588 patients with LVO treated with TNK 0.25 mg/kg showed that pre-EVT recanalization occurred in 20.4% of patients, and these rates were similar in patients arriving directly at a CSC as well as transfers from primary stroke centers [27]. A physician survey comprising of 225 physicians from 44 countries showed that in current practice, 90% of respondents would offer IVT to patients with LVO stroke eligible for both IVT and EVT, and that 61% of participants would choose to use TNK over alteplase as the preferred drug for IVT if both drugs are backed by evidence. The focus group of patient participants identified a need to better understand patient characteristics that may benefit from EVT-only or combined strategies. These findings illustrate the fact that we need further studies with TNK amongst various patient subgroups to better inform decision-making [28]. A recently presented subgroup analysis of LVO population from AcT trial showed numerically better outcome (mRS 0–1) in TNK vs. alteplase (32.7% vs. 29.1%) with statistically significant better outcomes in internal carotid artery occlusions with TNK (26.1% vs. 18.2%) [29]. With results of AcT trial [8] potentially changing guidelines, the question of bridging using TNK in comparison to direct EVT remains unresolved. The DIRECT-TNK (Randomization to Endovascular Treatment Alone or Preceded by Systemic Thrombolysis With Tenecteplase in Ischemic Stroke; NCT05199194) study is an ongoing RCT aiming to answer this clinically relevant question.
Mobile stroke units
Although the EXTEND IA trials enrolled patients in mobile stroke units (MSUs), the analysis from MSU stratum has not been published separately. Currently, TASTE-A (Tenecteplase Versus Alteplase for Stroke Thrombolysis Evaluation Trial in the Ambulance) is the only published study which has tested TNK in the setting of mobile stroke units. This was a phase II RCT tested whether TNK (0.25 mg/kg) was superior to alteplase when administered in the setting of an MSU. The study included 104 patients (55 in TNK and 49 in alteplase arm) with median NIHSS of 8 at baseline presenting within 4.5 hours of symptom onset to the MSU in Melbourne, Australia. The primary outcome was the extent of perfusion lesion on CT perfusion imaging upon arrival at the receiving hospital. The study showed that on arrival at the hospital patients treated with TNK had a significantly smaller perfusion lesion (median 12 mL [interquartile range 3–28]) than with alteplase (35 mL [18–76]; adjusted incidence rate ratio 0.55, 95% CI 0.37–0.81; P=0.0030). For secondary outcomes, patients receiving TNK were treated significantly faster (median of 7 minutes) than those treated with alteplase and an mRS of 5 or 6 at 90 days was reported in eight (15%) patients allocated to TNK and ten (20%) patients allocated to alteplase (adjusted OR 0.70, 95% CI 0.23–2.16; P=0.54). No cases of SICH were reported within 36 hours with either treatment [11]. This study provides preliminary evidence to support the use of TNK and MSUs in an optimal model of stroke care. The AcT study which randomized some of the patients in MSU would add more evidence in this field, when published.
Current guidelines
While practice is already changing, guidelines still focus primarily on alteplase. The current American Heart Association/American Stroke Association (2019) guidelines give a grade IIB recommendation to consider 0.25 mg/kg of TNK over intravenous alteplase in patients who are also eligible for EVT, based on the data from the EXTEND-IA TNK trial [30]. European guidelines (2021) provide a weak recommendation suggesting that TNK could be considered over alteplase in patients with ischemic stroke presenting within 4.5 hours of onset who are ineligible for EVT, as well as in patients with LVO, citing a low quality of evidence [31]. The Canadian guidelines do not comment on the use of TNK [32]. Lastly, the Australian guidelines recommend strongly to use either TNK or alteplase in patients presenting with LVO stroke [33]. Table 2 shows a summary of future and current ongoing trials.
Conclusion
TNK has emerged as a promising alternative to alteplase in the treatment of acute ischemic stroke, with compelling data from several trials regarding its relative safety and efficacy. The newer trial results have helped to address important gaps between the current state of evidence and this data may help in revising international guidelines on the use of TNK in ischemic stroke.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2022.02880.
Notes
Disclosure
The authors have no financial conflicts of interest.
Acknowledgements
None


