 |
 |
- Search
| J Stroke > Volume 25(2); 2023 > Article |
|
Abstract
The collateral circulation plays a crucial role in maintaining perfusion to brain tissue in ischemic stroke, which prolongs the time window for effective therapies to be provided and ultimately avoids irreversible damage that may lead to worse clinical outcomes. The understanding of this complex vascular bypass system has advanced greatly in the past few years, yet effective treatments for its potentiation as a therapeutic target remain a challenge. The assessment of the collateral circulation is now part of the routine neuroimaging protocols for acute ischemic stroke, which provides a more complete pathophysiological picture in each patient that allows for a better selection for acute reperfusion therapies and a more accurate prognostication of outcomes, among other potential uses. In this review, we aim to provide a structured and updated approach to the collateral circulation while highlighting ongoing research areas with promising future clinical applications.
Ischemic stroke is up to this day a leading cause of morbidity and mortality worldwide [1]. The presence of penumbra (i.e., potentially salvageable brain tissue that is at risk of progressing to infarct) is at the center of the rationale for providing acute reperfusion therapies, namely intravenous thrombolysis and endovascular procedures. Classically, the “time is brain” paradigm has been used and, accordingly, time windows for these treatments have been established. This concept emphasizes the idea that the faster the reperfusion is achieved, the higher the chances of preserving viable brain tissue will be, which ultimately improves functional outcomes. On the other hand, a later treatment might be futile because there is no significant volume of tissue to salvage and the chance of treatment-associated complications progressively increases with time. These concepts have been proven by sub-analyses of previous trials, which have shown a time-dependent benefit of acute reperfusion therapies even within the established time windows for treatment [2-5].
The widespread use of advanced neuroimaging has led to a better understanding of the dynamics of the progression of brain tissue from penumbra to infarct, to a better selection of patients for acute reperfusion therapies, and ultimately to the current ongoing expansion of the criteria to select patients for these treatments. The paradigm has accordingly been shifting from a time-oriented to a tissue-oriented approach. In this regard, the collateral circulation plays a critical role in sustaining viable brain tissue for longer periods and in allowing for reperfusion therapies to be given at later times. The “collateral clock” concept has accordingly been suggested [6]. Moreover, the collateral circulation can play several other roles in ischemic stroke and it has therefore emerged as a prognostic marker, a factor to consider when selecting patients for acute treatments, and a potential treatment target.
A deep understanding of the anatomy, physiology, pathophysiology, evaluation methods, clinical applications, and potential enhancement methods of the brain collateral circulation allows clinicians to provide better care for their patients with ischemic stroke and to contribute to the ever-growing knowledge in this field. In a previous review [7], these different aspects were analyzed; however, important advances in knowledge have been made during the past decade and, thus, we believe that an updated review is warranted.
The collateral circulation of the brain refers to alternative or indirect arterial pathways that can potentially provide blood flow when an artery that normally supplies an area of brain tissue is occluded (Table 1).
From a structural point of view, these pathways can be broadly divided into three anatomical categories (Figure 1).
The circle of Willis (CoW) is a ring of interconnected mediumsized arteries located at the base of the brain (Figure 1C). It connects the anterior and posterior circulations and the left and right hemispheres. The CoW can provide immediate diversion of blood flow in the case of an acute occlusion of a parent vessel. An important caveat is that the CoW has many possible variations and less than 50% of patients have a complete, symmetrical, and well-developed circle. These variations may significantly affect the capacity of the CoW to provide collateral pathways of blood flow and they have been shown to impact outcomes in ischemic stroke (Figure 2) [7,8].
Carotid terminus occlusions are illustrative of the collateral potential of the CoW. These occlusions can take several forms (i.e., I-type, L-type, and T-type) with each having different patterns of collateralization [9]. The Willisian collateral status can also help predict outcomes in these patients [10].
Apart from the posterior communicating arteries, the persistent carotid-vertebrobasilar anastomoses are other possible connections between the anterior and posterior circulations. These arteries are present during the embryonic period and they usually involute, but they may rarely persist into adult life [8].
These are small arteriolar connections (approximately 50-400 µm) at the distalmost branches of large cerebral and cerebellar vessels (Figure 1A and B). These connections display variable configurations including end-to-end and end-to-side anastomoses. Blood can flow in both directions through these anastomoses as a function of the hemodynamic and metabolic needs of the territories they connect [7].
If an occlusion of an intracranial vessel occurs, the leptomeningeal anastomoses can provide retrograde flow from the distal cortical areas of the territory of the occluded vessel (Figure 3).
The current available information shows that collateral formation and maturation is a complex process which involves several genes and pathways.
Collaterogenesis, or the formation of leptomeningeal collaterals, occurs during the embryonic period (Figure 4). Murine models have identified a locus on chromosome 7 whose allelic variants explain more than 80% of the variation in collateral extent. This locus has been called Determinant of collateral extent-1 (Dce1). The Rab GTPase-effector binding protein 2 (Rabep2) gene was subsequently identified as the causative allele at Dce1 [11]. Rabep2 is ubiquitously expressed and is involved in vascular endothelial growth factor-A (VEGF-A)/vascular endothelial growth factor receptor 2 (VEGFR2) signaling through vesicular trafficking [12]. Collateral formation is impaired in Rabep2-/- embryos. Mutations of Rabep2 do not affect pre- or postnatal development and growth of the general arterial-venous vasculature, capillary density, normal or tumor angiogenesis, or any other apparent phenotype other than collateral abundance [13]. Paracrine VEGF-A activates flk1 (VEGFR2) and initiates delta-like ligand 4 (Dll4) binding to Notch on adjacent endothelial cells. Dll4 is a transmembrane ligand of Notch receptors, selectively expressed in arterial and angiogenic tip cells during development. Its binding to Notch promotes a “tip cell” phenotype in an endothelial cell of a distal-most arteriole of the cerebral artery tree. A disintegrin and metalloprotease (ADAM) 10 and gamma-secretase cleavage activity are required for Notch intracellular domain (NCID) signaling and promotion of a “stalk cell” phenotype in the trailing endothelial cells. This endothelial sprouting process ultimately leads to the fusion of a terminal arteriole to an opposing arteriole, thus forming a new collateral [14,15]. Dll4-Notch signaling restricts pial collateral artery formation during embryogenesis. Dll4 heterozygous mice show an increased number of pial collaterals compared to littermates, but with no variation in the volume of infarcted tissue in middle cerebral artery (MCA) occlusion models and with no variation in outcomes in hindlimb ischemia models. These results suggest that not only the number of collaterals is important but also their functionality [16]. Apart from pathways involved in formation of pial collaterals, other pathways involved in their maturation have been studied. Chloride intracellular channel-4 (CLIC4) has a positive effect in collateral maturation while the endothelial-specific ephrin type-A receptor 4 (EphA4) has a suppressing effect on pial collateral remodeling [16,17]. Findings from murine models require further confirmation in humans.
The prevailing notion that small subcortical infarcts, with their different possible mechanisms, are caused by the occlusion of terminal penetrating arteries which lack collateral pathways has been challenged. There is evidence from post-mortem human studies of the presence of anastomoses between major perforator arteries and precapillary arterioles. Also, more recent studies using computed tomography (CT) and magnetic resonance (MR) perfusion techniques have provided indirect evidence of the presence of both anterograde and retrograde collaterals in small subcortical infarcts (Figure 1A and B). This suggests that the core-penumbra model may also be applied to this type of infarcts [18,19].
There are several possible extra-intracranial anastomoses, which can provide blood flow in the case of a blood vessel occlusion. These extracranial sources originate from branches of the external carotid artery or from ascending and deep cervical arteries (Figure 1D) [7].
One example is an occlusion of the internal carotid artery (ICA) before the emergence of the ophthalmic artery. If there is a complete and functional CoW, the terminal ICA may receive retrograde flow through the circle and immediately restore the anterograde flow through the ophthalmic artery. If there is insufficient collateral circulation through the CoW, another possible source of blood flow are branches of the external carotid artery, which can anastomose with branches of the ophthalmic artery and provide retrograde flow, which will ultimately reach the terminal ICA [20].
From a functional point of view, the collateral circulation can be divided into primary, secondary, and tertiary types.
The primary collateral circulation corresponds to permanently functioning pathways that can immediately reroute blood flow when a blood vessel occlusion occurs. This term refers mainly to the CoW.
The secondary collateral circulation refers to pre-existing arterial conduits that can instantaneously be recruited to provide an alternative pathway for blood flow. This refers mainly to the leptomeningeal collaterals. The recruitment of leptomeningeal collaterals is extremely fast. For example, in rat models of ICA occlusion, it takes only 12 seconds for leptomeningeal collaterals to reach their maximal vasodilatation [21].
There are several neurohumoral mechanisms involved in the process of leptomeningeal collateral recruitment. The main driver of the functionality of these pathways is pressure gradients [22]. It is important to keep in mind that in the context of an acute large vessel occlusion (LVO) the cerebral autoregulation is impaired and blood flow through collateral arteries becomes particularly dependent on the mean arterial pressure. In this sense, the resistance of the collateral network plays a determinant role. Shear stress through these vessels activates nitric oxide (NO)-dependent mechanisms that lead to their dilation and improved blood flow. There is also a neural regulation of the cerebrovascular tone through intrinsic (i.e., from the central nervous system) and extrinsic (i.e., from the peripheral nervous system) innervations. The intrinsic nerves originate mainly in the brainstem and are distributed predominantly in the parenchymal vessels, whereas the extrinsic nerves supply the vessels on the surface of the brain [23]. The extrinsic parasympathetic nerves, which arise from the superior salivatory nucleus and pass along cranial nerve VII to the sphenopalatine and otic ganglia, are involved in vasodilation and their stimulation has been studied as a therapeutic target. Several neurotransmitters are involved in these pathways, such as acetylcholine, vasoactive intestinal polypeptide, peptide histidine isoleucine and nitrous oxide [7].
Even though the extent and functionality of the collateral circulation in adulthood is largely determined by collaterogenesis and its implicated genes and pathways, it can also be modified throughout the patient’s life by several factors.
Aging causes a decrease in number and diameter and an increase in tortuosity of leptomeningeal collaterals, which lead to increased vascular resistance. These changes are associated with impaired endothelial NO synthase (eNOS) signaling and increased oxidative stress. In a retrospective analysis of 70 patients with proximal MCA occlusion, every 10-year increment in age increased the odds of having poor collaterals by a factor of 1.87 (95% confidence interval [CI] 1.18-2.97) [24].
These are frequent comorbidities in stroke patients and they may have negative effects on the collateral circulation. In animal models of chronic hypertension, induction of collateral flow during acute ischemic stroke is impaired. This is associated with highly vasoconstricted pial collaterals that respond to pressure myogenically [25]. Clinical studies have suggested that chronic hypertension has a detrimental effect on collateral flow in patients with LVO. This detrimental effect is highest in those with untreated hypertension and lowest in those without hypertension, while hypertensive patients treated with antihypertensive medications are in between [26]. Similarly, murine models of common carotid artery occlusion have shown impaired collateral flow in diabetic mice [27]. Previous reports from patients with coronary artery disease have suggested that smoking may be associated with better collaterals. The proposed mechanism is ischemic preconditioning; however, a 2021 meta-analysis of 18 studies and more than 4,000 patients did not demonstrate a positive association [28]. In the case of ischemic stroke, a retrospective analysis of embolic LVO in more than 600 patients found a positive correlation between smoking (current or previous) and good collaterals (odds ratio [OR] 1.74, CI 1.17-2.61, P=0.006) [29]. In a retrospective analysis of 206 consecutive patients with an M1 segment occlusion, multivariate analysis found the metabolic syndrome, hyperuricemia, and older age to be independent predictors of poor collaterals at baseline [30].
Regular exercise has been shown to improve collateral circulation in patients with coronary artery disease and in animal models of stroke. Physical exercise increases blood flow and the shear stress stimulates different mechanisms in the endothelium, which lead to maintenance, defense, and repair of the vasculature. It also enhances the capacity of the vessels to vasodilate. Another more indirect effect of physical exercise is the reduction of vascular risk factors [31].
Multiple observational studies have shown an association between previous statin use and better collaterals in ischemic stroke patients. Proposed mechanisms for this effect are enhancement of arteriogenesis and eNOS-mediated vasodilation. However, a 2019 meta-analysis of previous studies only showed a positive trend towards better collaterals. No differences between stroke subtypes were demonstrated [32].
In an observational study of 385 patients who underwent mechanical thrombectomy for LVO, patients with an ipsilateral stenosis of the extracranial ICA of more than 75% had an OR of 4.01 for having good collaterals (95% CI 1.78-9.00; P=0.001) [33].
The term tertiary collaterals is sometimes used to refer to the formation of new blood vessels or the maturation of pre-existent vessels in ischemic areas [34]. Two main processes are involved. Angiogenesis is the physiologic process in which new blood vessels arise from pre-existent ones. The main stimuli for angiogenesis are ischemia and hypoxia. In contrast, arteriogenesis refers to the maturation of pre-existent arterioles into arteries. It is an important process of adaptation of blood vessels to new demands from tissue at risk after an arterial occlusion. The main stimulus for arteriogenesis is the shear stress on the endothelium, which is generated by pressure gradients [35]. These processes take a longer time to develop, and thus their role is mainly in the context of chronic vascular occlusions. An illustrative example of tertiary collaterals is the moyamoya vessels that develop in patients with moyamoya disease and syndrome.
The main role of the collateral circulation is to maintain blood flow to the tissue that is normally supplied by an occluded vessel. This slows down the progression of tissue from penumbra to infarct, thus increasing the therapeutic time window, decreasing the final stroke volume, and decreasing the risk of hemorrhagic transformation [36]. The rate of progression from penumbra to infarct greatly depends on the extent of the collateral circulation and ultimately determines whether the patient will be a fast or a slow progressor. The persistence of blood flow to the blood clot also enhances the delivery of endogenous or exogenous tissue plasminogen activator, which increases the recanalization rate and decreases the re-occlusion rate. Likewise, in the case that potential neuroprotective agents are used, the collateral circulation can also enhance their delivery to brain tissue.
A functional venous drainage system is also important in ischemic stroke and it can enhance the function of the arterial collaterals. The possible roles of the venous system in this context can be broadly divided into the maintenance of sufficient collateral perfusion via adequate drainage of blood and clearance of microemboli, and the reduction of reperfusion injury [37].
The methods to assess the collateral circulation can be broadly divided into structural and functional types; however, there may be overlap in the type of information that they can provide.
These are imaging studies that visualize blood vessels and give an insight of the status of the collateral circulation either by static or dynamic acquisitions, but the actual anatomical connections are not necessarily seen.
Digital subtraction angiography (DSA) is considered the gold standard for structural assessment of the collateral circulation. This technique allows for the dynamic evaluation of blood flow with an excellent spatial and temporal resolution. It allows the assessment of the three main anatomical collateral pathways: the CoW, the extra-intracranial anastomoses, and the leptomeningeal collaterals. Its main disadvantages are its invasive nature, its associated procedural risks, the need for contrast agent administration, and its limited availability.
These are the most frequently used studies in the assessment of the collateral circulation because of their widespread availability and the brief additional time needed to perform them.
Single-phase CT angiography (sCTA), which is performed at a single time point in relation to the contrast bolus injection, has the limitation of being a static evaluation and can therefore provide an inexact measurement of the state of collaterals if the acquisition is not performed at the optimal time point. For example, in patients with a diminished cardiac ejection fraction or an extracranial carotid stenosis, the collaterals may be underestimated because the image acquisition will tend to be performed before the contrast agent can reach the leptomeningeal vessels. Previous studies have suggested that collateral assessment in sCTA in the early arterial and late venous phases underestimate and overestimate the collateral status, respectively. Probably the optimal timing for collateral grading on sCTA is in the peak arterial to equilibrium phase [38]. The collateral filling distal to a vascular occlusion may be better visualized on post-processed maximum intensity projection images [39].
Multiphase CTA (mCTA) is performed in different time points and provides a better characterization of the collateral circulation than sCTA because it allows the assessment of the delay in contrast arrival and washout. This technique also has a better interrater reliability for the detection of LVO, it allows for a more precise assessment of the thrombus length, and it has a better association with final infarct volume and clinical outcomes. mCTA requires brief extra time to be performed and it does not require additional contrast injection when compared to sCTA. At our institution, we routinely perform mCTA in three time points and rate the collaterals as described by Menon et al. [40] (Figure 5).
These techniques have well-known advantages over CT-based methods but they are not as readily available and they are usually slower to perform. However, advances in hardware and the development of novel imaging techniques have decreased acquisition times and thus MR-based protocols for acute imaging of stroke are becoming more commonly used [41].
Time-of-flight MR angiography (TOF-MRA) is a T1-based sequence that does not require gadolinium injection and is used to assess the proximal intracranial vasculature. It is based on blood flow which generates a visible signal. Its disadvantages are the acquisition time (approximately 5 minutes) and poor resolution of distal vessels. Also, slow flow distal to the occlusion can generate a complete loss of signal, which leads to an overestimation of the areas of occlusion. A significant advantage of TOF-MRA is that it can easily be reformatted into three-dimensional images because of its volumetric acquisition method [39].
Contrast-enhanced MR angiography (CE-MRA) is also a T1-based sequence and it requires the injection of a bolus of gadolinium. Its advantages are a high signal-to-noise ratio and a relative insensitivity to slow flow [42].
The fluid-attenuated inversion recovery (FLAIR) sequence can also provide information about collateral circulation. Vascular hyperintensities represent a more indirect marker of leptomeningeal collaterals, but they are non-specific and their usefulness is limited. The location of these hyperintensities in relation to the ischemic area is probably associated with the cerebral hemodynamic status. It has been observed that patients who have vascular hyperintensities only inside the ischemic area have worse collaterals when compared to patients who have vascular hyperintensities outside the ischemic area [43]. In a systematic review and meta-analysis of patients with ischemic strokes, FLAIR vascular hyperintensities as a whole were not associated with functional outcomes but an association was demonstrated for the subgroups of patients who underwent endovascular treatment and for those who had hyperintensities outside the ischemic territory [44].
This non-invasive method provides real-time information about intracranial blood flow. It only allows the assessment of proximal blood vessels at the level of the CoW, and it is an operator-dependent method. One possible finding is the inversion of blood flow through the ophthalmic artery or the A1 segment of the anterior cerebral artery (ACA) in the context of an ipsilateral distal ICA occlusion. Another possible finding is the flow diversion phenomenon, which refers to the findings of high velocity and low resistance in the ipsilateral ACA and/or posterior cerebral artery (PCA) in the context of an MCA occlusion. This is associated with the presence of anastomoses between the distal branches of the ACA/PCA and the MCA. These findings have shown a sensitivity of 81% and a specificity of 76% when compared with DSA for the presence of leptomeningeal collaterals [45].
Tissue perfusion studies allow for the assessment of the compensation by the collateral circulation.
CT perfusion (CTP) is widely available, fast, and together with non-contrast CT and CTA is a part of the multimodal acute stroke neuroimaging protocol in many centers, including ours (Figure 5). In this technique, multiple acquisitions of the brain parenchyma are performed during contrast infusion. As the contrast flows through the brain, the increase, peak and decrease of density are captured in a time-density curve, which allows for the calculation of different perfusion parameters [39]. In particular, the volume of ischemic core and penumbra can be calculated using standardized definitions. These measurements are routinely used to select patients for acute reperfusion therapies.
Different softwares may be employed for the processing of perfusion images, such as the rapid processing of perfusion and diffusion (RAPID) software (IschemaView, Menlo Park, CA, USA) which is routinely used at our center and which also employs artificial intelligence (AI) technology to detect LVOs. CTP studies usually require an additional dose of contrast agent. Interestingly, the StrokeSENS™ software (Circle Neurovascular Imaging, Calgary, AB, Canada) allows perfusion studies to be performed from mCTA images without the need of an additional dose of contrast agent and it can also perform AI-based automated Alberta Stroke Program Early CT Score (ASPECTS) scoring from non-contrast CT images and LVO detection from CTA images. This software is available for clinical use in the EU, UK, Canada, Australia, and USA but only for LVO detection, with the rest of the features currently reserved for research purposes [46]. There are several other AI-based softwares that can perform automated interpretation of neuroimaging in acute stroke [47].
CTP can also be helpful in estimating the rate of progression from penumbra to ischemic core and thus in differentiating between fast and slow progressors, which can have implications in management and prognosis of acute stroke patients with LVO. The hypoperfusion index (HI) was first described in 2008 and is now preferably calculated as the ratio of time-to-peak concentration at >10 seconds divided by time-to-peak concentration at >6 seconds. In a cohort of medium-vessel-occlusion and LVO patients, an HI >0.5 versus ≤0.5 accurately differentiated fast from slow progressors, respectively, in the first 24 hours of an ischemic stroke (Figure 6) [48].
There are several possible clinical situations that may produce false positive and false negative results in CTP studies, so their results should always be interpreted considering the clinical picture and the concomitant vascular imaging. Some examples of these situations are migraine aura, seizures, and large vessel stenosis which can alter the local hemodynamic balance.
Similar to CTP, in MR perfusion-weighted imaging (PWI), the signal intensity of the brain is measured at different intervals while a contrast agent is administered intravenously. Perfusion parameters can be calculated from the time-concentration curve after deconvolution [49]. However, in the case of MR-based studies, the infarct core is most accurately estimated not by perfusion parameters but by diffusion-weighted imaging (DWI), which shows areas of cytotoxic edema only minutes after the onset of ischemia. DWI is more sensitive for the detection of acute ischemia than CT-based methods, especially for small subcortical infarcts. DWI-PWI mismatch is routinely used in MR-based studies to determine the area of penumbra [50,51].
Tissue perfusion studies can also be performed with positron emission tomography CT and single-photon emission CT, but these are mostly reserved for investigation purposes. They can be combined with a vasodilator stimulus, such as in the acetazolamide challenge test, to assess the cerebrovascular reserve in a given patient [52].
Arterial spin labeling (ASL) is an MR-based technique that provides a quantitative measurement of cerebral blood flow (CBF) and it has the advantage of not requiring the administration of a contrast agent. It can also provide structural information of pial collaterals, which can be visualized as linear hyperintense regions of increased CBF in the periphery of the area of ischemic penumbra. Despite its advantages, ASL has not gained widespread use in stroke for several reasons, most importantly for its high sensitivity to differences in arterial arrival time which may ultimately lead to an overestimation of CBF and an underestimation of tissue at risk. These shortcomings might be mitigated by methodological improvements [53,54]. The presence of collaterals detected by ASL are correlated with good clinical outcomes in retrospective series of patients with acute ischemic stroke. The Imaging Collaterals in Acute Stroke (iCAS) is an ongoing prospective cohort study of patients undergoing ASL imaging before mechanical thrombectomy and it is evaluating the relationship between pre-treatment collateral status and response to thrombectomy and functional outcomes [39]. This information might be valuable for the potential addition of ASL into MR-based imaging protocols in acute ischemic stroke.
The methods to assess the collateral circulation that we have mentioned so far imply the presence of a large vessel stenosis or occlusion that ultimately causes the pial collateral channels to be open (i.e., to be recruited). However, having a non-invasive imaging biomarker of the collateral status before a vessel occlusion or stroke occurs is a current need because it would provide valuable information for understanding the physiology and pathophysiology of the collateral circulation during a patient’s life, it could serve as a prognostic marker, and it would also help evaluate potential early therapeutic strategies of collateral circulation augmentation.
Retinal vessel metrics have been proposed as a surrogate marker of leptomeningeal collateral status. Retinal fundus images have previously been used to identify alterations in the retinal vasculature to predict stroke and it has been observed that retinal vessel width differs between stroke subtypes and between patients with recurrent strokes. Murine models of acute ischemic stroke have identified several retinal vessel parameters that predict the pial collateral status, infarct volume, and neurological outcomes. A recent translational human study showed that standard retinal vessel metrics such as venular widening and lower arterio-venular ratio and tortuosity differ in patients with acute ischemic stroke when compared to healthy controls, but they do not differentiate patients with good from those with poor pial collaterals. On the other hand, increased retinal vessel multifractal dimensions were shown to be a marker of poor pial collaterals in patients with acute ischemic stroke. These findings need to be confirmed on larger studies, and the usefulness of these metrics in patients with intra- or extracranial vascular stenosis or occlusion prior to ischemic stroke remains to be explored [55].
Numerous scales have been created to standardize the evaluation of the collateral circulation. They are based on the different available study methods and use different criteria to grade the extent of collaterals [39]. Several of them dichotomize the grading into good and poor collaterals. The variable use of these different scales can make it difficult to compare studies regarding the collateral circulation and its different possible clinical uses. Moreover, the concordance between different modalities has been shown to be poor [56]. A recent pooled analysis of patient-level data from the Highly Effective Reperfusion evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration comparing three different collateral scales showed that a regional collateral scale on sCTA provided the most accurate prediction of functional outcome, while on time-resolved CTA there were no differences among the different scales [38]. Automated methods based on AI are promising techniques to improve and standardize the evaluation of the collateral circulation; however, their use is currently only approved for investigational purposes [47].
Given the importance of a functional venous drainage system and its complementary and synergistic nature with the arterial collateral system in the context of acute ischemic stroke, scales that grade the venous drainage either by itself or in combination with an arterial collateral grading system have been devised. Several of these scales have shown a significant association with outcomes and complications such as hemorrhagic transformation [57-61]. These findings suggest that venous collateral grading might be used as an additional imaging biomarker for outcome prediction and possibly treatment selection in acute stroke patients.
Intracranial atherosclerotic disease (ICAD) is a major etiology of stroke, especially in patients of certain ethnicities. ICAD can cause strokes by several mechanisms, one of them being hypoperfusion secondary to progressive stenosis. In such cases, the longstanding ischemia may lead to the progressive recruitment or development of collaterals as opposed to an acute embolic occlusion [62]. In line with these pathophysiological mechanisms, previous studies have reported a possible role of collateral status observation either by structural or functional methods in determining the etiology of stroke [63-65]. A recent meta-analysis in patients with acute stroke receiving reperfusion therapies found that large artery atherosclerosis etiology was associated with a significantly increased rate of pre-treatment good collaterals (risk ratio [RR] 1.24; 95% CI 1.04-1.50; P=0.020) when compared to cardioembolic etiology, but with heterogeneity between studies [66].
Poor collaterals on admission are associated with a larger ischemic core and worse clinical outcomes [67]. In the first 48 hours of an ischemic stroke, the presence of good collaterals is associated with early clinical improvement. Patients with poor collaterals have higher frequency of hemorrhagic transformation, both symptomatic and asymptomatic [68]. In a large prospective cohort of patients with LVO, the presence of good collaterals was an independent predictor of good long-term outcomes, and this effect was more evident if they did not receive reperfusion therapies. In a large cohort of patients with LVO and multimodal CT imaging, it was noted that the collateral status is not consistently associated with the size of the penumbra, but it is associated with the core volume and its growth speed [69,70].
In the case of ICAD, the association of good collaterals with better outcomes may not be valid because in these cases the occurrence of a stroke might represent an exhaustion of the collateral system. However, there is scarce data to support this notion and more information is needed [60]. In a retrospective analysis of the Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) trial the quality of collaterals independently predicted the occurrence of new strokes in the symptomatic territory [71].
In a systematic review and meta-analysis which included 25 retrospective cohorts and 3 post-hoc analyses of randomized controlled trials (RCTs) and a total of 3,057 patients, those with good collaterals had a lower risk of symptomatic hemorrhagic transformation (RR 0.38; 95% CI 0.16-0.90; P=0.03), a higher frequency of early neurological improvement (RR 4.21; 95% CI 1.57-11.28, P=0.004), a higher frequency of good clinical outcomes (modified Rankin Scale [mRS] 0-2) at 3-6 months (RR 2.45; 95% CI 1.94-3.09; P<0.001), a lower National Institutes of Health Stroke Scale (NIHSS) on admission (median difference of 6 points), and a smaller infarct volume on admission. There were no statistically significant results associated with collateral status for successful recanalization and reperfusion, global risk of hemorrhagic transformation, final infarct volume, and mortality at 3 months [72].
In two systematic reviews and meta-analyses which included studies that were published until March 2015, good collaterals before the endovascular procedure were significantly associated with a higher frequency of successful reperfusion as measured by the modified Thrombolysis in Cerebral Infarction (mTICI) score (RR=1.28; 95% CI 1.17-1.40; P<0.001), a higher frequency of successful recanalization as measured by the Arterial Occlusive Lesion (AOL) score (RR=1.23; 95% CI 1.06-1.42; P=0.006), a higher frequency of good funcional outcome (mRS≤2) at 90 days (RR=1.98, 95% CI 1.64 to 2.38; P<0.001), a reduced risk of periprocedural symptomatic intracranial hemorrhage (sICH) (RR=0.59; 95% CI 0.43 to 0.81; P=0.001) and death at 90 days (RR=0.49; 95% CI 0.38 to 0.63; P<0.001) [73,74]. Table 2 shows studies published after March 2015 that reported the association of collateral status and outcomes in patients treated with endovascular thrombectomy (EVT) for anterior circulation LVO stroke [40,75-92]. A similar analysis for vertebrobasilar LVO can be found in a recent review, showing conflicting results [93].
The latest American Heart Association/American Stroke Association guidelines suggest that it may be reasonable to incorporate collateral flow status into clinical decision-making in some candidates to determine eligibility for mechanical thrombectomy with a IIb level of evidence. No specific criteria are suggested [95].
Considering the overall ominous functional prognosis in patients with pre-procedure poor collaterals, one may make a case for excluding these patients from EVT. However, it must be kept in mind that the number of patients in previous analyses was small and that probably the collateral status is one more of several factors that should be considered when making such a decision [79].
We may highlight some special groups of patients when considering the collateral status as a factor to select or exclude patients from acute reperfusion therapies.
There are several ongoing trials to assess the effectiveness and safety of EVT in patients with a low baseline ASPECTS. The collateral status may be an important factor to consider when selecting these patients. In a retrospective analysis of 100 patients with LVO and ASPECTS ≤5 who were treated with EVT, a good collateral status and younger age (<73 years) were associated with better functional outcomes [96].
A pooled analysis of late window EVT studies compared patients selected using collateral status plus perfusion imaging (current standard criteria) with those selected using collateral status only. They found no significant difference in functional outcomes at 3 months, but sICH was twice more frequent in the collateral only group with no significant difference in mortality at 3 months [97]. There are currently two ongoing trials evaluating patient selection for late window EVT with CT and CTA which could provide more insight into this issue: Randomization of Endovascular Treatment in Acute Ischemic Stroke in the Extended Time Window (RESILIENTExt, NCT04256096; Brazil) and Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands for Late Arrivals (MR CLEAN-LATE, ISRCTN19922220; Netherlands). Such approaches that do not require CTP might help us expand the access to EVT.
There is limited data evaluating the safety and efficacy of very late window EVT, but well-selected patients might benefit from this treatment, highlighting the importance of a tissue-based approach rather than a time-based approach to acute reperfusion therapies. A trial to assess EVT beyond 24 hours will probably require a collaborative approach from multiple centers given the low number of patients that might be eligible [98-100]. Assessment of the collateral circulation might also be an important factor to consider when selecting these patients.
The optimal blood pressure (BP) management strategy in the peri-EVT period is an ongoing area of research. Enhancing the collateral perfusion before recanalization and avoiding reperfusion damage and hemorrhagic transformation after recanalization are of utmost importance to achieve better functional outcomes. Patients with better collaterals might have better tolerance to BP fluctuations and it has been shown that poor baseline collaterals can aggravate the deleterious effects of higher BP levels or higher BP variability on clinical outcomes [101].
The Efficacy Study of Combined Treatment With Uric Acid and rtPA in Acute Ischemic Stroke (URICO-ICTUS) trial was an RCT in patients treated with intravenous thrombolysis to assess the administration of uric acid before the thrombolytic infusion was completed. The trial was negative for the primary outcome of better functional outcome at 3 months. In a posterior nested study that divided the patients by collateral status, only those with excellent collaterals had significantly better functional outcomes after the administration of uric acid. This example emphasizes the possible role of collaterals in the delivery of potential neuroprotective agents to the ischemic tissue [102].
Several treatment options to enhance the collateral circulation have previously been tested in clinical trials. Currently, none of these strategies have demonstrated a clear benefit to recommend their regular use. However, several of them have had promising results, and there are ongoing trials trying to prove their benefit.
The management of ICAD can be challenging, especially when best medical therapy fails. The use of invasive procedures in this situation raises the concern for associated adverse events.
Encephaloduroarteriosynangiosis (EDAS) is an indirect extracranial-intracranial (EC-IC) bypass surgical technique, which is most described as a treatment option for patients with moyamoya disease/syndrome. The EDAS Revascularization for Symptomatic Intracranial Atherosclerotic Steno-occlusive (ERSIAS) trial was a phase-II single-arm trial in patients with symptomatic ICAD (>70% stenosis in the intracranial ICA or M1 segment) and failure to best medical therapy. It compared EDAS plus intensive medical therapy versus intensive medical therapy alone. They found a reduction of any stroke or death in the first 30 days or any stroke in the territory of the affected vessel thereafter, reaching the non-futility threshold for advancement to a phase-III trial, with only mild surgical complications and no ICH. A post-hoc analysis of the trial, which only considered patients with borderzone infarcts, which are considered to have a higher risk of recurrence, found a significant reduction of the primary endpoint. A phase-III trial is expected [103].
Ischemic conditioning is a technique that consists of producing transient ischemia—but not necrosis—in a tissue. It can be performed directly, e.g., on a coronary artery, or remotely, e.g., on a limb. It is believed that it activates endogenous protective pathways in distant organs such as the kidney, the heart, and the brain via humoral, immune, and neural mechanisms [104]. Remote ischemic conditioning (RIC) can be applied as preconditioning (i.e., before the ischemic event), perconditioning (e.g., during the ischemic event), or postconditioning (i.e., after the ischemic event).
RIC has been evaluated in acute myocardial infarction, where it has demonstrated a reduction in infarcted tissue in ST-segment elevation myocardial infarction patients, but with no benefit in clinical outcomes [105]. In the case of ischemic stroke, clinical studies have not revealed a clear benefit to recommend its use. There is low-quality evidence suggesting that postconditioning might have a beneficial effect on clinical and neuroimaging outcomes [106,107]. There are several ongoing trials of RIC in acute ischemic stroke [105,108,109].
RIC is a simple, low-cost, and safe treatment, so the demonstration of its benefit could easily lead to widespread implementation.
As we mentioned before, the stimulation of the extrinsic parasympathetic pathway has an effect on the intracranial vasculature. Specifically, pre-clinical and physiological studies have determined at least four mechanisms by which the stimulation of the sphenopalatine ganglion (SPG), a parasympathetic ganglion located in the pterygopalatine fossa, could be beneficial in ischemic stroke: vasodilation with the subsequent increase in blood flow through collateral pathways, stabilization of the bloodbrain barrier, neuroprotection via central cholinergic and adrenergic pathways, and enhancement of neuroplasticity [110].
The stimulation of the SPG through an implantable device has been tested in the injectable implant to stimulate the sphenopalatine ganglion for treatment of acute ischaemic stroke (ImpACT) trials, but they failed to show a significant benefit in the intention to treat population. However, they did demonstrate a significant benefit as an improvement beyond expectation in the mRS in the subgroup of patients with a confirmed cortical infarct, highlighting the importance of adequate patient selection [111].
Capsaicin (8-methyl-N-vanillyl-trans-6-nonenamide)—a component of hot chili peppers—is being investigated as a non-invasive alternative for the stimulation of the SPG. In a pilot study performed in healthy volunteers, oral capsaicin showed a dose-dependent augmentation of the MCA mean velocity and diminution of the pulsatility index on transcranial Doppler [112].
NO donors are candidate neuroprotective agents in acute ischemic stroke. Due to their vasodilator effects, they are postulated to produce a potentiation of collateral circulation and a decrease in blood pressure. Nitroglycerin is a systemic NO donor and vasodilator. Its transdermal administration has been tested in the context of acute ischemic and hemorrhagic stroke, but no clinical benefit has been demonstrated when given within 6 hours of symptom onset [113]. It has been suggested that an earlier administration of nitroglycerin may provide clinical benefit; however, recently the prehospital transdermal glyceryl trinitrate in patients with presumed acute stroke (Multicenter Randomized trial of Acute Stroke treatment in the Ambulance with a nitroglycerin Patch [MR ASAP]) trial failed to demonstrate a clinical benefit of this treatment when applied within 3 hours of symptom onset in the prehospital setting. Interestingly, the study suggested a possible harm in ICH patients, in whom we might have suspected that the BP lowering effects would have been beneficial [114].
PP-007 (previously Sanguinate™, SG) is a PEGylated carboxyhemoglobin (PEG-COHb) gas transfer agent with pleiotropic effects on the brain and cerebral circulation. Its protective effects are thought to be mediated by several mechanisms, including vasodilation. Preclinical studies have demonstrated decreased neurological deficits, reduced infarct volume, and collateral enhancing properties of SG. There is an ongoing phase 1 multicenter clinical trial for treatment of LVO in patients undergoing endovascular thrombectomy (Safety Study of PP-007 in Subjects With Acute Ischemic Stroke [HEMERA-1]) [25].
Rapamycin is an inhibitor of mammalian target of rapamycin, which has been shown to be neuroprotective in animal models of stroke. In a rat model of stroke, rapamycin increased collateral perfusion during MCA occlusion and reperfusion. The observed dilation of leptomeningeal anastomoses was abolished by NOS inhibition, suggesting NO release as a mechanism of collateral enhancement by rapamycin. Currently, no clinical trials of rapamycin in acute ischemic stroke are ongoing [25,115].
TM5441 is a selective inhibitor of plasminogen activator inhibitor-1. It has a vasodilator effect that is mediated through NO release. In a rat model of stroke, the infusion of TM5441 increased collateral perfusion and reduced early infarct. Currently, no clinical trials of TM5441 in acute ischemic stroke are ongoing [25,116].
Significant advances in the field of brain collateral circulation research have been made in the past few years. Our understanding of this complex bypass system during all stages of life in both healthy and morbid states is ever-growing, yet still incomplete. There is robust evidence to support the idea that the collateral circulation is a major determinant of outcomes in ischemic stroke and thus effective strategies to potentiate it are a current necessity.
Early interventions to potentiate the collateral circulation and avoid its rarefaction with age and other comorbid factors may have a significant impact in patients with acute stroke. In this regard, a deeper understanding of collaterogenesis and the factors that impact the collateral circulation across a patient’s life might reveal new potential intervention strategies. Assessment methods of the collateral circulation before a stroke occurs are also a necessity in the development and evaluation of these early intervention strategies.
More comprehensive scales that consider not only the arterial bypass routes but also the importance of the venous drainage system, and also a standardization of assessment methods is needed to better assess this complex system and to simplify communication and collaboration in research and daily clinical practice. Automated AI-based softwares are a promising tool for this purpose.
Safe and effective methods for acute potentiation of the collateral circulation in the context of acute ischemic stroke are also important, given that this will most likely remain the most common situation in which we might potentially intervene.
Figure 1.
Schematic representation of the collateral circulation of the brain. The anterior circulation is represented in dark red, the posterior circulation in light red, and the extracranial sources of blood flow in orange. (A) Antero-posterior and (B) lateral view of the main intracranial arteries. The persistent carotid-vertebrobasilar anastomoses are represented with a dashed dark red line. (C) Inferior view of the circle of Willis and a corresponding diagram showing each arterial component. (D) Lateral view of cranio-cervical arteries highlighting the main extra-intracranial anastomoses. Microvascular anastomoses between (1) the anterior cerebral artery (ACA) and the middle cerebral artery (MCA), (2) the ACA and the posterior cerebral artery (PCA), (3) the MCA and the PCA, and (4) the superior cerebellar artery and the posterior inferior cerebellar artery. (5) The postulated collateral pathways in the deep subcortical territory. Extra-intracranial anastomoses between (6) branches of the facial artery and the ophthalmic artery, (7) the supraorbital and supratrochlear arteries and branches of the ophthalmic artery, (8) branches of the occipital artery and the PCA, (9) the middle meningeal artery and the ACA, and (10) branches from ascending and deep cervical arteries and the vertebral artery. AcommA, anterior communicating artery; R A1, A1 segment of the right ACA; L A1, A1 segment of the left ACA; R ICA, right internal carotid artery; L ICA, left internal carotid artery; R PcommA, right posterior communicating artery; L PcommA, left posterior communicating artery; R P1, P1 segment of the right PCA; L P1, P1 segment of the left PCA; BA, basilar artery.
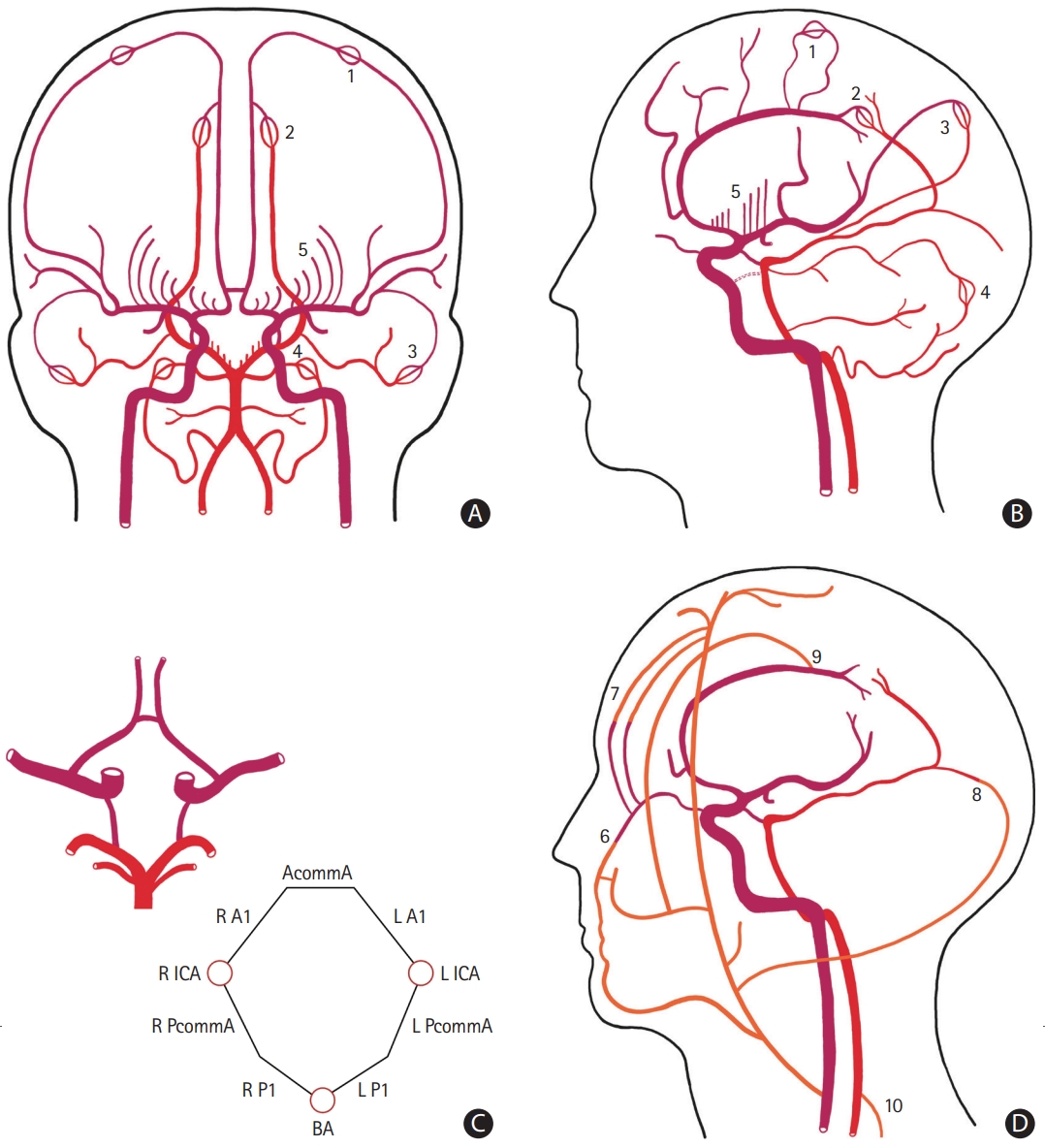
Figure 2.
Axial maximum intensity projection computed tomography angiography slices showing examples of circle of Willis (CoW) configurations. (A) A complete CoW. (B) A CoW with absence of the left posterior communicating artery (arrow).
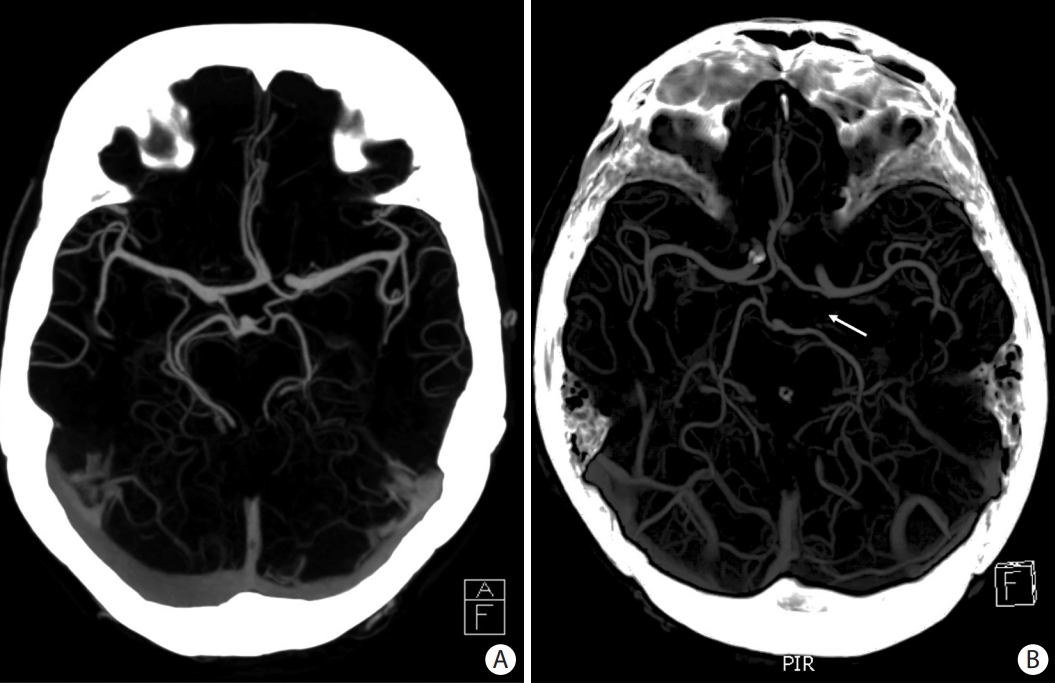
Figure 3.
Sequential antero-posterior images in digital subtraction angiography after contrast injection in the right internal carotid artery in a patient with an occlusion of the M1 segment of the right middle cerebral artery (arrow). Notice the contrast filling of the left anterior circulation through the anterior communicating artery (dashed arrow) in the earliest image. The direction of the blood flow through the leptomeningeal collaterals from anterior cerebral artery to middle cerebral artery is shown with a curved arrow.

Figure 4.
Collaterogenesis occurs during the embryonic period. (A) The differentiation of endothelial cells into tip and stalk phenotypes is dependent on vascular endothelial growth factor (VEGF)/vascular endothelial growth factor receptor 2 (VEGFR2) signaling. (1) Rabep2, whose genetic variations largely determine the differences on collateral extent in murine models, promotes the Rab4 recycling of VEGFR2 to the cell surface, increasing its availability. (2) VEGF binding to VEGFR2 induces endocytosis and signaling which (3) induces delta-like ligand 4 (Dll4). (4) Dll4 activates the transmembrane receptor Notch1, of which the Notch intracellular domain (NICD) is liberated and (5) induces several effects in the adjacent stalk cells, such as cell division. (B) Tip cells are guided by the VEGF gradient and direct the growing sprout while stalk cells follow behind and form the vascular lumen. This process leads to the fusion of two terminal arterioles, forming a new collateral. In the example, a new collateral is forming between terminal branches of the anterior cerebral artery (ACA) to middle cerebral artery (MCA). Rabep2, Rab GTPase-effector binding protein 2; Rab4, Rab GTPase 4.
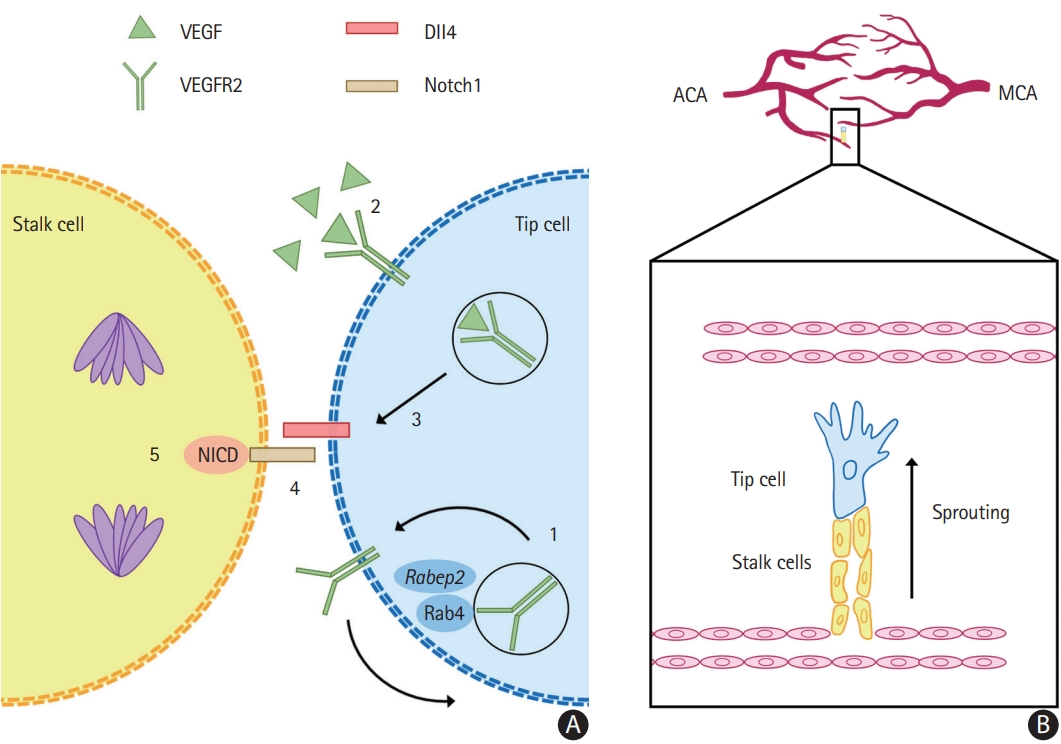
Figure 5.
Examples of patients with acute large vessel occlusion (LVO) and their respective computed tomography agiography (CTA) and computed tomography perfusion studies. Each row sequentially shows axial maximum intensity projection images of the LVO and the three phases of CTA, followed by the ischemic core (defined as cerebral blood flow [CBF] <30% of contralateral side) and penumbra (defined as time-to-maximum [Tmax] >6 s) images with their respective automated volume calculation. (A) Left “T occlusion” (distal internal carotid artery, A1 and M1 segments, arrow) with good collaterals. Notice the filling of the left A2 segment from the contralateral side (dashed arrow). (B) Left M1 occlusion (arrow) with moderate collaterals. (C) Left “T occlusion” (arrow) with poor collaterals. Notice the retrograde filling of the left A1 segment and left posterior communicating artery (dashed arrows).
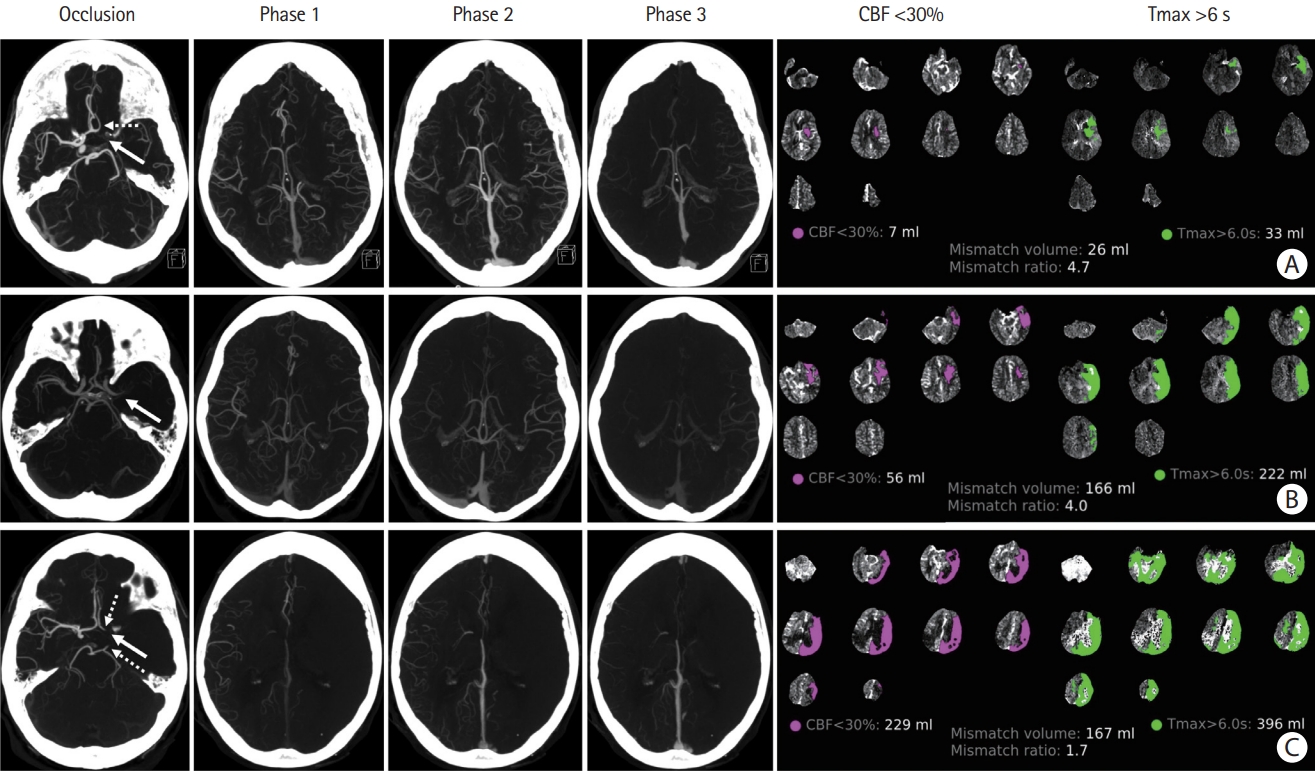
Figure 6.
The hypoperfusion index (HI=Tmax>10 s/Tmax>6 s) in fast versus slow progressors. (A) Fast progressor: patient with an acute left “L occlusion” (distal internal carotid artery extending into the middle cerebral artery [MCA], arrow) with imaging performed 90 minutes after onset of symptoms. HI=0.6. (B) Slow progressor: patient with an acute right MCA occlusion (arrow) with imaging performed 120 minutes after onset of symptoms. HI=0.2. CBF, cerebral blood flow.
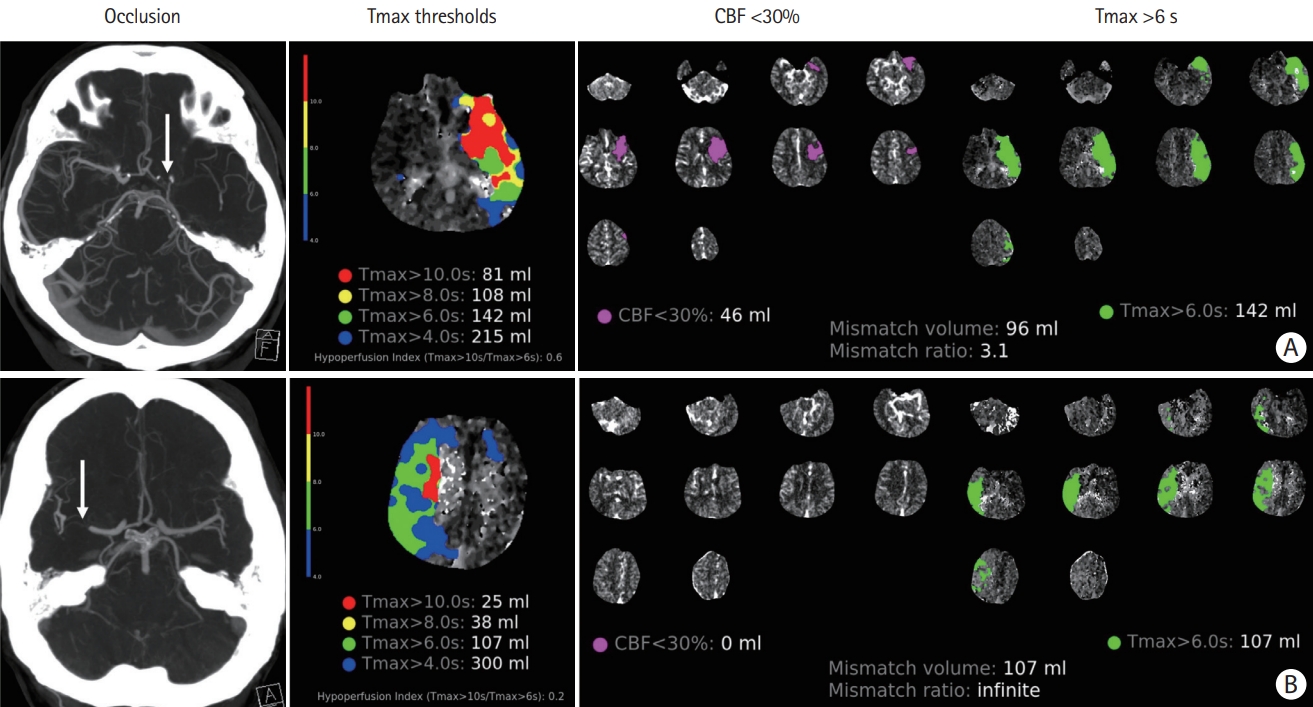
Table 1.
Overview of the collateral circulation of the brain
Table 2.
Selected studies reporting the association between pre-treatment collateral status and outcomes after EVT of anterior circulation large vessel occlusion stroke
| Study | Patients (n) | Collateral scale (method) | Main findings |
|---|---|---|---|
| Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke trials (HERMES) collaboration [75] | 1,764 (871 EVT, 893 control) | Tan et al. [76] (sCTA, mCTA, or CE-MRA) | Analyses suggested benefit with EVT across all strata of collateral circulation status; however, patients with poor collaterals were less likely to benefit from EVT than those with better collaterals (not statistically significant). |
| Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke (DEFUSE 3) trial [77] | 130 (65 EVT, 65 control) | Tan et al. [76] (sCTA, mCTA, or CE-MRA) | No significant association with good clinical outcome*, sICH, or death. Good collaterals were associated with significantly smaller ischemic core volume and less ischemic core growth. |
| Diffusion-Weighted Imaging or Computed Tomography Perfusion Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) trial [92] | 161 (91 EVT, 70 control) | Tan et al. [76] (CTA) | Significant association between collateral status and infarct core at 24 h, ASPECTS at 24 h, successful revascularization (eTICI ≥2b), good functional outcome*, and death. |
| ASITN/SIR [78] (DSA) | |||
| Gerber et al. [79] | 93 | Tan et al. [76] | Good collaterals were significantly associated with good clinical outcome* (OR 9.69; 95% CI 2.28-59.27; P=0.001). |
| Sedation versus Intubation for Endovascular Stroke TreAtment (SIESTA) trial [80] | 104 | Tan et al. [76] | Good collaterals were significantly associated with smaller final infarct volume, improvement in the mean NIHSS at 24 h, and in-house mortality. No significant association was found with functional outcome or 3-month mortality. |
| Sallustio et al. [81] | 135 | Tan et al. [76] (CTA) | Significant association between good collaterals and good functional outcome* (OR 2.13; 95% CI 1.44 to 3.15; P<0.001), lower mortality rate, lower rate of sICH, higher ASPECTS at 24 h, and higher NIHSS improvement at 24 h. |
| Christoforidis et al. [82] (DSA) | |||
| Park et al. [83] | 119 | Regional colateral scoring system [84] | Good collaterals were an independent predictor of good functional outcome* (OR 5.14; 95% CI 1.62-16.26; P=0.005). |
| Renú et al. [85] | 339 (257 EVT, 82 no EVT) | Tan et al. [76] | The benefit of EVT (reduction in infarct growth, functional outcome, and mortality) was significantly higher in patients with poor collaterals. |
| Weiss et al. [86] | 84 | Tan et al. [76] (sCTA) | Good collaterals in the Miteff and Maas scores were significantly associated with good functional outcome*. |
| Miteff et al. [87] (sCTA) | |||
| Maas et al. [88] (sCTA) | |||
| Al-Dasuqi et al. [89] | 283 | Miteff et al. [87] (sCTA) | Collateral grade was significantly associated with final infarct volume but not with functional outcome. |
| Optimizing Patient’s Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) study [90] | 361 (285 EVT, 76 medical management) | mCTA [40] | Collateral status was significantly associated with early infarct growth rate which in turn was significantly associated with functional outcome. |
| Endovascular Treatment in Ischemic Stroke (ETIS) Registry [91] | 2,020 | ASITN/SIR (DSA) | Good collaterals were associated with successful reperfusion (OR 1.77; 95% CI 1.32-2.39; P<0.001), excellent reperfusion (OR 1.71; 95% CI 1.41-2.09; P<0.001), and good functional outcome* (OR 1.5; 95% CI 1.19-1.88; P<0.001), but not with sICH or mortality at 3 months. |
EVT, endovascular thrombectomy; sCTA, single-phase computed tomography angiography; mCTA, multiphase computed tomography angiography; CE-MRA, contrast-enhanced magnetic resonance angiography; sICH, symptomatic intracranial hemorrhage; CTA, computed tomography angiography; ASITN/SIR, American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology scale; DSA, digital subtraction angiography; ASPECTS, Alberta Stroke Program Early CT Score; eTICI, expanded Thrombolysis in Cerebral Infarction; OR, odds ratio; CI, confidence interval; NIHSS, National Institutes of Health Stroke Scale; mRS, modified Rankin Scale.
References
1. Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke 2022;17:18-29.



2. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929-1935.



3. Bourcier R, Goyal M, Liebeskind DS, Muir KW, Desal H, Siddiqui AH, et al. Association of time from stroke onset to groin puncture with quality of reperfusion after mechanical thrombectomy: a meta-analysis of individual patient data from 7 randomized clinical trials. JAMA Neurol 2019;76:405-411.



4. Almekhlafi MA, Goyal M, Dippel DWJ, Majoie CBLM, Campbell BCV, Muir KW, et al. Healthy life-year costs of treatment speed from arrival to endovascular thrombectomy in patients with ischemic stroke: a meta-analysis of individual patient data from 7 randomized clinical trials. JAMA Neurol 2021;78:709-717.

5. Ma G, Yu Z, Jia B, Xian Y, Ren Z, Mo D, et al. Time to endovascular reperfusion and outcome in acute ischemic stroke: a nationwide prospective registry in China. Clin Neuroradiol 2022;32:997-1009.



6. Vagal A, Aviv R, Sucharew H, Reddy M, Hou Q, Michel P, et al. Collateral clock is more important than time clock for tissue fate. Stroke 2018;49:2102-2107.



7. Shuaib A, Butcher K, Mohammad AA, Saqqur M, Liebeskind DS. Collateral blood vessels in acute ischaemic stroke: a potential therapeutic target. Lancet Neurol 2011;10:909-921.


8. Harrigan MR, Deveikis JP. Essential neurovascular anatomy. In : Harrigan MR, Deveikis JP, editors. Handbook of Cerebrovascular Disease and Neurointerventional Technique Totowa, NJ: Humana Press; 2013. p. 3-98.
9. Malhotra K, Goyal N, Tsivgoulis G. Internal carotid artery occlusion: pathophysiology, diagnosis, and management. Curr Atheroscler Rep 2017;19:41.



10. Lee SU, Hong JM, Kim SY, Bang OY, Demchuk AM, Lee JS. Differentiating carotid terminus occlusions into two distinct populations based on Willisian collateral status. J Stroke 2016;18:179-186.




11. Lucitti JL, Sealock R, Buckley BK, Zhang H, Xiao L, Dudley AC, et al. Variants of rab GTPase-effector binding protein-2 cause variation in the collateral circulation and severity of stroke. Stroke 2016;47:3022-3031.



12. Kofler N, Corti F, Rivera-Molina F, Deng Y, Toomre D, Simons M. The Rab-effector protein RABEP2 regulates endosomal trafficking to mediate vascular endothelial growth factor receptor-2 (VEGFR2)-dependent signaling. J Biol Chem 2018;293:4805-4817.



13. Zhang H, Faber JE. Transient versus permanent MCA occlusion in mice genetically modified to have good versus poor collaterals. Med One 2019;4:e190024.


14. Lucitti JL, Mackey JK, Morrison JC, Haigh JJ, Adams RH, Faber JE. Formation of the collateral circulation is regulated by vascular endothelial growth factor-A and a disintegrin and metalloprotease family members 10 and 17. Circ Res 2012;111:1539-1550.



15. Mack JJ, Iruela-Arispe ML. NOTCH regulation of the endothelial cell phenotype. Curr Opin Hematol 2018;25:212-218.



16. Perovic T, Harms C, Gerhardt H. Formation and maintenance of the natural bypass vessels of the brain. Front Cardiovasc Med 2022;9:778773.



17. Okyere B, Mills WA 3rd, Wang X, Chen M, Chen J, Hazy A, et al. EphA4/Tie2 crosstalk regulates leptomeningeal collateral remodeling following ischemic stroke. J Clin Invest 2020;130:1024-1035.



18. Rudilosso S, Laredo C, Mancosu M, Moya-Planas N, Zhao Y, Chirife O, et al. Cerebral perfusion and compensatory blood supply in patients with recent small subcortical infarcts. J Cereb Blood Flow Metab 2019;39:1326-1335.




19. Huang YC, Lee JD, Pan YT, Weng HH, Yang JT, Lin LC, et al. Perfusion defects and collateral flow patterns in acute small subcortical infarction: a 4D dynamic MRI study. Transl Stroke Res 2022;13:399-409.




20. Costa VP, Kuzniec S, Molnar LJ, Cerri GG, Puech-Leão P, Carvalho CA. Collateral blood supply through the ophthalmic artery: a steal phenomenon analyzed by color Doppler imaging. Ophthalmology 1998;105:689-693.


21. Morita Y, Fukuuchi Y, Koto A, Suzuki N, Isozumi K, Gotoh J, et al. Rapid changes in pial arterial diameter and cerebral blood flow caused by ipsilateral carotid artery occlusion in rats. Keio J Med 1997;46:120-127.


22. Iwasawa E, Ichijo M, Ishibashi S, Yokota T. Acute development of collateral circulation and therapeutic prospects in ischemic stroke. Neural Regen Res 2016;11:368-371.



23. Hamel E. Perivascular nerves and the regulation of cerebrovascular tone. J Appl Physiol (1985) 2006;100:1059-1064.


24. Arsava EM, Vural A, Akpinar E, Gocmen R, Akcalar S, Oguz KK, et al. The detrimental effect of aging on leptomeningeal collaterals in ischemic stroke. J Stroke Cerebrovasc Dis 2014;23:421-426.


25. Cipolla MJ. Therapeutic induction of collateral flow. Transl Stroke Res 2022 Apr 13 [Epub]. https://doi.org/10.1007/s12975-022-01019-2.

26. Fujita K, Tanaka K, Yamagami H, Ide T, Ishiyama H, Sonoda K, et al. Detrimental effect of chronic hypertension on leptomeningeal collateral flow in acute ischemic stroke. Stroke 2019;50:1751-1757.


27. Nishijima Y, Akamatsu Y, Yang SY, Lee CC, Baran U, Song S, et al. Impaired collateral flow compensation during chronic cerebral hypoperfusion in the type 2 diabetic mice. Stroke 2016;47:3014-3021.



28. Pei J, Wang X, Xing Z. Traditional cardiovascular risk factors and coronary collateral circulation: a meta-analysis. Front Cardiovasc Med 2021;8:743234.



29. Vilanilam GK, Badi MK, McCoy EG, D’Souza CE, Becker TL, Miller DA, et al. Abstract TP127: impact of smoking on collateral blood flow in patients with acute ischemic stroke with large cerebral artery embolic occlusion. Stroke 2019;50(Suppl_1):ATP127.

30. Menon BK, Smith EE, Coutts SB, Welsh DG, Faber JE, Goyal M, et al. Leptomeningeal collaterals are associated with modifiable metabolic risk factors. Ann Neurol 2013;74:241-248.



31. Hung SH, Kramer S, Werden E, Campbell BCV, Brodtmann A. Pre-stroke physical activity and cerebral collateral circulation in ischemic stroke: a potential therapeutic relationship? Front Neurol 2022;13:804187.



32. Malhotra K, Safouris A, Goyal N, Arthur A, Liebeskind DS, Katsanos AH, et al. Association of statin pretreatment with collateral circulation and final infarct volume in acute ischemic stroke patients: a meta-analysis. Atherosclerosis 2019;282:75-79.


33. Pienimäki JP, Sillanpää N, Jolma P, Protto S. Carotid artery stenosis is associated with better intracranial collateral circulation in stroke patients. Cerebrovasc Dis 2020;49:200-205.



34. Liu L, Ding J, Leng X, Pu Y, Huang LA, Xu A, et al. Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol 2018;3:117-130.



35. Hendrikx G, Vöö S, Bauwens M, Post MJ, Mottaghy FM. SPECT and PET imaging of angiogenesis and arteriogenesis in preclinical models of myocardial ischemia and peripheral vascular disease. Eur J Nucl Med Mol Imaging 2016;43:2433-2447.




36. Bang OY, Goyal M, Liebeskind DS. Collateral circulation in ischemic stroke: assessment tools and therapeutic strategies. Stroke 2015;46:3302-3309.



37. Tong LS, Guo ZN, Ou YB, Yu YN, Zhang XC, Tang J, et al. Cerebral venous collaterals: a new fort for fighting ischemic stroke? Prog Neurobiol 2018. 163-164:172-193.



38. Gensicke H, Al-Ajlan F, Fladt J, Campbell BCV, Majoie CBLM, Bracard S, et al. Comparison of three scores of collateral status for their association with clinical outcome: the HERMES collaboration. Stroke 2022;53:3548-3556.


39. Heit JJ, Zaharchuk G, Wintermark M. Advanced neuroimaging of acute ischemic stroke: penumbra and collateral assessment. Neuroimaging Clin N Am 2018;28:585-597.

40. Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, et al. Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology 2015;275:510-520.


41. You SH, Kim B, Kim BK, Park SE. Fast MRI in acute ischemic stroke: applications of MRI acceleration techniques for MRbased comprehensive stroke imaging. Investig Magn Reson Imaging 2021;25:81-92.


42. Raymond SB, Schaefer PW. Imaging brain collaterals: quantification, scoring, and potential significance. Top Magn Reson Imaging 2017;26:67-75.

43. Huang X, Shi X, Yang Q, Zhou Y, Xu X, Xu J, et al. Topography of the hyperintense vessel sign on fluid-attenuated inversion recovery represents cerebral hemodynamics in middle cerebral artery occlusion: a CT perfusion study. Neuroradiology 2019;61:1123-1130.



44. Zhou Z, Malavera A, Yoshimura S, Delcourt C, Mair G, Al-Shahi Salman R, et al. Clinical prognosis of FLAIR hyperintense arteries in ischaemic stroke patients: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2020;91:475-482.


45. Guan J, Zhang S, Zhou Q, Li C, Lu Z. Usefulness of transcranial Doppler ultrasound in evaluating cervical-cranial collateral circulations. Interv Neurol 2013;2:8-18.




46. Circle Neurovascular Imaging. StrokeSENS [Internet]. Calgary, Canada: Circle Neurovascular Imaging [cited 2022 Aug 23]. Available from: https://www.circlenvi.com/.
47. Wardlaw JM, Mair G, von Kummer R, Williams MC, Li W, Storkey AJ, et al. Accuracy of automated computer-aided diagnosis for stroke imaging: a critical evaluation of current evidence. Stroke 2022;53:2393-2403.


48. Nomani AZ, Kamtchum Tatuene J, Rempel JL, Jeerakathil T, Winship IR, Khan KA, et al. Association of CT-based hypoperfusion index with ischemic core enlargement in patients with medium and large vessel stroke. Neurology 2021;97:e2079-e2087.



49. Kim BJ, Kang HG, Kim HJ, Ahn SH, Kim NY, Warach S, et al. Magnetic resonance imaging in acute ischemic stroke treatment. J Stroke 2014;16:131-145.



50. Bateman M, Slater LA, Leslie-Mazwi T, Simonsen CZ, Stuckey S, Chandra RV. Diffusion and perfusion MR imaging in acute stroke: clinical utility and potential limitations for treatment selection. Top Magn Reson Imaging 2017;26:77-82.

51. Demeestere J, Wouters A, Christensen S, Lemmens R, Lansberg MG. Review of perfusion imaging in acute ischemic stroke: from time to tissue. Stroke 2020;51:1017-1024.


52. Vagal AS, Leach JL, Fernandez-Ulloa M, Zuccarello M. The acetazolamide challenge: techniques and applications in the evaluation of chronic cerebral ischemia. AJNR Am J Neuroradiol 2009;30:876-884.



53. Zaharchuk G. Arterial spin labeling for acute stroke: practical considerations. Transl Stroke Res 2012;3:228-235.




54. Haller S, Zaharchuk G, Thomas DL, Lovblad KO, Barkhof F, Golay X. Arterial spin labeling perfusion of the brain: emerging clinical applications. Radiology 2016;281:337-356.


55. Khan A, De Boever P, Gerrits N, Akhtar N, Saqqur M, Ponirakis G, et al. Retinal vessel multifractals predict pial collateral status in patients with acute ischemic stroke. PLoS One 2022;17:e0267837.



56. Kauw F, Dankbaar JW, Martin BW, Ding VY, Boothroyd DB, van Ommen F, et al. Collateral status in ischemic stroke: a comparison of computed tomography angiography, computed tomography perfusion, and digital subtraction angiography. J Comput Assist Tomogr 2020;44:984-992.



57. Parthasarathy R, Kate M, Rempel JL, Liebeskind DS, Jeerakathil T, Butcher KS, et al. Prognostic evaluation based on cortical vein score difference in stroke. Stroke 2013;44:2748-2754.



58. Parthasarathy R, Sohn SI, Jeerakathil T, Kate MP, Mishra SM, Nambiar VK, et al. A combined arterial and venous grading scale to predict outcome in anterior circulation ischemic stroke. J Neuroimaging 2015;25:969-977.



59. Bala F, Singh N, Menon BK, Demchuk AM, Poppe AY, McTaggart RA, et al. Poor cortical venous opacification on baseline computed tomography angiography predicts parenchymal hemorrhage after thrombectomy. Stroke Vasc Interv Neurol 2022;2:e000299.

60. Winkelmeier L, Broocks G, Kniep H, Geest V, Reinwald J, Meyer L, et al. Venous outflow profiles are linked to clinical outcomes in ischemic stroke patients with extensive baseline infarct. J Stroke 2022;24:372-382.




61. Faizy TD, Mlynash M, Kabiri R, Christensen S, Kuraitis GM, Mader MM, et al. The cerebral collateral cascade: comprehensive blood flow in ischemic stroke. Neurology 2022 Apr 28 [Epub]. https://doi.org/10.1212/WNL.0000000000200340.

62. Leng X, Leung TW. Collateral flow in intracranial atherosclerotic disease. Transl Stroke Res 2022 Jun 8 [Epub]. https://doi.org/10.1007/s12975-022-01042-3.

63. Haussen DC, Bouslama M, Dehkharghani S, Grossberg JA, Bianchi N, Bowen M, et al. Automated CT perfusion prediction of large vessel acute stroke from intracranial atherosclerotic disease. Interv Neurol 2018;7:334-340.




64. Baek JH, Kim BM, Kim JW, Kim DJ, Heo JH, Nam HS, et al. Utility of leptomeningeal collaterals in predicting intracranial atherosclerosis-related large vessel occlusion in endovascular treatment. J Clin Med 2020;9:2784.



65. Sun D, Huo X, Ma N, Gao F, Mo D, et al. Prediction of intracranial atherosclerotic acute large vessel occlusion by severe hypoperfusion volume growth rate. J Stroke Cerebrovasc Dis 2022;31:106799.


66. Sinha A, Stanwell P, Beran RG, Calic Z, Killingsworth MC, Bhaskar SMM. Stroke aetiology and collateral Status in acute ischemic stroke patients receiving reperfusion therapy—a meta-analysis. Neurol Int 2021;13:608-621.



67. Ravindran AV, Killingsworth MC, Bhaskar S. Cerebral collaterals in acute ischaemia: implications for acute ischaemic stroke patients receiving reperfusion therapy. Eur J Neurosci 2021;53:1238-1261.



68. Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B, et al. Collateral flow averts hemorrhagic transformation after endovascular therapy for acute ischemic stroke. Stroke 2011;42:2235-2239.


69. Nannoni S, Cereda CW, Sirimarco G, Lambrou D, Strambo D, Eskandari A, et al. Collaterals are a major determinant of the core but not the penumbra volume in acute ischemic stroke. Neuroradiology 2019;61:971-978.



70. Lin L, Yang J, Chen C, Tian H, Bivard A, Spratt NJ, et al. Association of collateral status and ischemic core growth in patients with acute ischemic stroke. Neurology 2021;96:e161-e170.


71. Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ, et al. Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Ann Neurol 2011;69:963-974.



72. Leng X, Lan L, Liu L, Leung TW, Wong KS. Good collateral circulation predicts favorable outcomes in intravenous thrombolysis: a systematic review and meta-analysis. Eur J Neurol 2016;23:1738-1749.



73. Leng X, Fang H, Leung TW, Mao C, Xu Y, Miao Z, et al. Impact of collateral status on successful revascularization in endovascular treatment: a systematic review and meta-analysis. Cerebrovasc Dis 2016;41:27-34.



74. Leng X, Fang H, Leung TW, Mao C, Miao Z, Liu L, et al. Impact of collaterals on the efficacy and safety of endovascular treatment in acute ischaemic stroke: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2016;87:537-544.


75. Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol 2018;17:895-904.

76. Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol 2009;30:525-531.



77. de Havenon A, Mlynash M, Kim-Tenser MA, Lansberg MG, Leslie-Mazwi T, Christensen S, et al. Results from DEFUSE 3: good collaterals are associated with reduced ischemic core growth but not neurologic outcome. Stroke 2019;50:632-638.



78. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 2013;44:2650-2663.



79. Gerber JC, Petrova M, Krukowski P, Kuhn M, Abramyuk A, Bodechtel U, et al. Collateral state and the effect of endovascular reperfusion therapy on clinical outcome in ischemic stroke patients. Brain Behav 2016;6:e00513.



80. Schönenberger S, Pfaff J, Uhlmann L, Klose C, Nagel S, Ringleb PA, et al. The impact of conscious sedation versus general anesthesia for stroke thrombectomy on the predictive value of collateral status: a post hoc analysis of the SIESTA trial. AJNR Am J Neuroradiol 2017;38:1580-1585.



81. Sallustio F, Motta C, Pizzuto S, Diomedi M, Giordano A, D’Agostino VC, et al. CT angiography-based collateral flow and time to reperfusion are strong predictors of outcome in endovascular treatment of patients with stroke. J Neurointerv Surg 2017;9:940-943.


82. Christoforidis GA, Mohammad Y, Kehagias D, Avutu B, Slivka AP. Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 2005;26:1789-1797.


83. Park JS, Kwak HS, Chung GH, Hwang S. The prognostic value of CT-angiographic parameters after reperfusion therapy in acute ischemic stroke patients with internal carotid artery terminus occlusion: leptomeningeal collateral status and clot burden score. J Stroke Cerebrovasc Dis 2018;27:2797-2803.


84. Menon BK, O’Brien B, Bivard A, Spratt NJ, Demchuk AM, Miteff F, et al. Assessment of leptomeningeal collaterals using dynamic CT angiography in patients with acute ischemic stroke. J Cereb Blood Flow Metab 2013;33:365-371.




85. Renú A, Laredo C, Montejo C, Zhao Y, Rudilosso S, Macias N, et al. Greater infarct growth limiting effect of mechanical thrombectomy in stroke patients with poor collaterals. J Neurointerv Surg 2019;11:989-993.


86. Weiss D, Kraus B, Rubbert C, Kaschner M, Jander S, Gliem M, et al. Systematic evaluation of computed tomography angiography collateral scores for estimation of long-term outcome after mechanical thrombectomy in acute ischaemic stroke. Neuroradiol J 2019;32:277-286.




87. Miteff F, Levi CR, Bateman GA, Spratt N, McElduff P, Parsons MW. The independent predictive utility of computed tomography angiographic collateral status in acute ischaemic stroke. Brain 2009;132(Pt 8):2231-2238.


88. Maas MB, Lev MH, Ay H, Singhal AB, Greer DM, Smith WS, et al. Collateral vessels on CT angiography predict outcome in acute ischemic stroke. Stroke 2009;40:3001-3005.



89. Al-Dasuqi K, Payabvash S, Torres-Flores GA, Strander SM, Nguyen CK, Peshwe KU, et al. Effects of collateral status on infarct distribution following endovascular therapy in large vessel occlusion stroke. Stroke 2020;51:e193-e202.



90. Sarraj A, Hassan AE, Grotta J, Blackburn S, Day A, Abraham M, et al. Early infarct growth rate correlation with endovascular thrombectomy clinical outcomes: analysis from the SELECT study. Stroke 2021;52:57-69.


91. Anadani M, Finitsis S, Clarençon F, Richard S, Marnat G, Bourcier R, et al. Collateral status reperfusion and outcomes after endovascular therapy: insight from the endovascular treatment in ischemic stroke (ETIS) Registry. J Neurointerv Surg 2022;14:551-557.


92. Liebeskind DS, Saber H, Xiang B, Jadhav AP, Jovin TG, Haussen DC, et al. Collateral circulation in thrombectomy for stroke after 6 to 24 hours in the DAWN trial. Stroke 2022;53:742-748.


93. Lee SJ, Hong JM, Kim JS, Lee JS. Endovascular treatment for posterior circulation stroke: ways to maximize therapeutic efficacy. J Stroke 2022;24:207-223.




94. Voleti S, Aziz YN, Vidovich J, Corcoran B, Zhang B, Mistry E, et al. Association between CT angiogram collaterals and CT perfusion in delayed time windows for large vessel occlusion ischemic strokes. J Stroke Cerebrovasc Dis 2022;31:106263.


95. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019;50:e344-e418.


96. Broocks G, Kniep H, Schramm P, Hanning U, Flottmann F, Faizy T, et al. Patients with low Alberta Stroke Program Early CT Score (ASPECTS) but good collaterals benefit from endovascular recanalization. J Neurointerv Surg 2020;12:747-752.


97. Almekhlafi MA, Thornton J, Casetta I, Goyal M, Nannoni S, Herlihy D, et al. Stroke imaging prior to thrombectomy in the late window: results from a pooled multicentre analysis. J Neurol Neurosurg Psychiatry 2022;93:468-474.


98. Manning NW, Wenderoth J, Alsahli K, Cordato D, CappelenSmith C, McDougall A, et al. Endovascular thrombectomy >24-hr from stroke symptom onset. Front Neurol 2018;9:501.



99. Dhillon PS, Butt W, Podlasek A, Barrett E, McConachie N, Lenthall R, et al. Endovascular thrombectomy beyond 24 hours from ischemic stroke onset: a propensity score matched cohort study. J Neurointerv Surg 2022 Feb 15 [Epub]. https://doi.org/10.1136/neurintsurg-2021-018591.

100. Purrucker JC, Ringleb PA, Seker F, Potreck A, Nagel S, Schönenberger S, et al. Leaving the day behind: endovascular therapy beyond 24h in acute stroke of the anterior and posterior circulation. Ther Adv Neurol Disord 2022;15:17562864221101083.




101. Kim BJ, Singh N, Menon BK. Hemodynamics of leptomeningeal collaterals after large vessel occlusion and blood pressure management with endovascular treatment. J Stroke 2021;23:343-357.




102. Amaro S, Renú A, Laredo C, Castellanos M, Arenillas JF, Llull L, et al. Relevance of collaterals for the success of neuroprotective therapies in acute ischemic stroke: insights from the randomized URICO-ICTUS trial. Cerebrovasc Dis 2019;47:171-177.



103. Gonzalez NR, Jiang H, Lyden P, Song S, Schlick K, Dumitrascu O, et al. Encephaloduroarteriosynangiosis (EDAS) revascularization for symptomatic intracranial atherosclerotic stenoocclusive (ERSIAS) phase-II objective performance criterion trial. Int J Stroke 2021;16:701-709.



104. Hess DC, Blauenfeldt RA, Andersen G, Hougaard KD, Hoda MN, Ding Y, et al. Remote ischaemic conditioning-a new paradigm of self-protection in the brain. Nat Rev Neurol 2015;11:698-710.



105. Saccaro LF, Aimo A, Emdin M, Pico F. Remote ischemic conditioning in ischemic stroke and myocardial infarction: similarities and differences. Front Neurol 2021;12:716316.



106. Zhao JJ, Xiao H, Zhao WB, Zhang XP, Xiang Y, Ye ZJ, et al. Remote ischemic postconditioning for ischemic stroke: a systematic review and meta-analysis of randomized controlled trials. Chin Med J (Engl) 2018;131:956-965.


107. An JQ, Cheng YW, Guo YC, Wei M, Gong MJ, Tang YL, et al. Safety and efficacy of remote ischemic postconditioning after thrombolysis in patients with stroke. Neurology 2020;95:e3355-e3363.


108. Abuduxukuer R, Guo ZN, Zhang P, Qu Y, Yang Y. Safety and efficacy of remote ischemic conditioning combined with intravenous thrombolysis for acute ischemic stroke: a multicenter, randomized, parallel-controlled clinical trial (SERICIVT) study design and protocol. Int J Stroke 2022 Jul 5 [Epub]. https://doi.org/10.1177/17474930221104991.

109. Guo ZN, Abuduxukuer R, Zhang P, Wang C, Yang Y. Safety and efficacy of remote ischemic conditioning combined with endovascular thrombectomy for acute ischemic stroke due to large vessel occlusion of anterior circulation: a multicenter, randomized, parallel-controlled clinical trial (SERIC-EVT): study protocol. Int J Stroke 2022 Sep 12 [Epub]. https://doi.org/10.1177/17474930221121429.

110. Bahr-Hosseini M, Saver JL. Mechanisms of action of acute and subacute sphenopalatine ganglion stimulation for ischemic stroke. Int J Stroke 2020;15:839-848.



111. Baker TS, Robeny J, Cruz D, Bruhat A, Iloreta AM, Costa A, et al. Stimulating the facial nerve to treat ischemic stroke: a systematic review. Front Neurol 2021;12:753182.



112. Marquez-Romero JM, Huerta-Franco MR, Vargas-Luna M, Madrigal-Gutiérrez CA, Esparza-Hernández JM, Velázquez-Barcena MG. Dose escalation and safety of capsaicin for cerebral perfusion augmentation: a pilot study. Stroke 2021;52:2203-2209.


113. Lim BL, Lee WF, Ng WM, Situ W, Loo KV, Man Goh CJ, et al. Benefits and safety of transdermal glyceryl trinitrate in acute stroke: a systematic review and meta-analysis of randomized trials. Acad Emerg Med 2022;29:772-788.



114. van den Berg SA, Uniken Venema SM, Reinink H, Hofmeijer J, Schonewille WJ, Miedema I, et al. Prehospital transdermal glyceryl trinitrate in patients with presumed acute stroke (MR ASAP): an ambulance-based, multicentre, randomised, open-label, blinded endpoint, phase 3 trial. Lancet Neurol 2022;21:971-981.

-

-
Smartphone App in Stroke Management: A Narrative Updated Review2023 May;25(2)
Smartphone App in Stroke Management: A Narrative Updated Review2022 September;24(3)
Anger, a Result and Cause of Stroke: A Narrative Review2022 September;24(3)
Posterior Circulation Stroke: Advances in Understanding and Management2021 January;23(1)







