Antiplatelet Therapy May Be Insufficient to Prevent Stroke Recurrence Before Percutaneous Patent Foramen Ovale Closure
Article information
Dear Sir:
Percutaneous patent foramen ovale (PFO) closure with antiplatelet (AP) therapy is superior to antithrombotic therapy alone for secondary prevention of cryptogenic stroke (CS) in patients with PFO (PFO-CS) [1-4]. Anticoagulant (AC) therapy is recommended for patients with venous thromboembolism (VTE), and even in patients without VTE, AC therapy, rather than AP therapy, may be considered [5,6]. AP therapy is started immediately after stroke onset until the causes of stroke are identified, particularly in patients without VTE. However, because AP therapy alone is associated with higher rates of stroke recurrence than PFO closure [1-4], we are concerned that AP therapy may be insufficient for preventing recurrence before PFO closure. We hypothesized that stroke recurrence is more common during AP therapy than during AC therapy before PFO closure.
This was a single-center, retrospective, observational study. The Institutional Review Board in our institute approved this study (IRB number 1108-01) and waived written informed consent due to its retrospective nature. Of 793 patients with ischemic stroke from April 2019 to September 2022, 22 patients (2.7%) who were diagnosed with PFO-CS and who underwent PFO closure to prevent stroke recurrence were evaluated.
PFO-CS patients with VTE are treated with AC therapy, and those without or undetected VTE are treated with AP therapy based on a guideline [5]. If the patient has a recurrent stroke during AP therapy, the patient may be switched to AC. Thorough diagnostic investigation, including 24-hour Holter electrocardiographic monitoring, transthoracic echocardiography, transesophageal echocardiography, carotid ultrasound, and magnetic resonance angiography (and/or computed tomography angiography), yielded no definitive cardioembolic source or arterial stenotic lesions. Transesophageal echocardiography with microbubble test were mandatory for the diagnosis of PFO. High-risk PFO was defined as a large PFO (with ≥20 microbubbles) and/or atrial septum aneurysm/hypermobile atrial septum. Stroke recurrence was defined as symptomatic and/or asymptomatic recurrence detected on diffusion-weighted imaging before PFO closure. The Risk of Paradoxical Embolism (RoPE) score [7] was calculated.
To clarify the relationship between stroke recurrence and antithrombotic therapy, the patients with no stroke recurrence were assigned to the non-recurrence group. In patients with stroke recurrence, if a patient had recurrence during AP and not after changing to AC, it was considered one recurrence during AP and one non-recurrence during AC (Figure 1). The RoPE score in the recurrence group was recalculated as having a previous stroke. Multivariate logistic regression analysis was performed to identify the factors associated with stroke recurrence. Variables of P<0.1 in the univariate analysis were included in the multivariate model. Because the RoPE score is a confounding factor with age and other risk factors, they were analyzed in separate models. The rate of recurrent stroke was plotted with the use of the Kaplan-Meier method.

Flowchart of inclusion and outcomes of the enrolled patients. The patients without stroke recurrence were assigned to the non-recurrence group. For patients with stroke recurrence, if the recurrence occurred during AP therapy and did not recur after changing to AC therapy, it was counted as 1 patient in the recurrence group and 1 patient in the non-recurrence group. Therefore, there were 6 patients in the recurrence group* and 20 patients in the no recurrence group†. PFO, patent foramen ovale; PFO-CS, cryptogenic stroke associated with PFO; AP, antiplatelet; AC, anticoagulant.
Of the total of 22 patients (median age, 56 years), 12 (55%) were men, their median RoPE score was 7 (range 2–10), and 20 (91%) had high-risk PFO (large PFO, 20 [91%]; atrial septum aneurysm/hypermobile atrial septum, 14 [64%]). The duration between index stroke and PFO closure was 153 days (interquartile range, 84–326 days). Five of 22 patients had recurrent stroke before PFO closure (23%, 1 patient had two recurrences), and 4 patients receiving an AP therapy were switched to AC therapy after recurrence. Therefore, the recurrence group included 6 patients, the non-recurrence group included 20 patients (Figure 1), and 5 of 12 patients on AP therapy (42%) had a recurrent stroke.
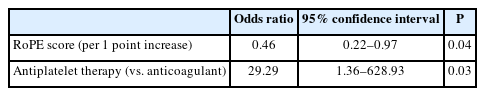
Patients in the recurrence group were older (age 67 vs. 52 years, P=0.03), had lower RoPE scores (3 vs. 7, P=0.03), and received AP therapy more often (83% vs. 35%, P=0.07) than those in the non-recurrence group (Table 1). None had stroke recurrence after PFO closure. Multivariate logistic regression analysis showed that low RoPE score (odds ratio [OR], 0.46; 95% confidence interval [CI], 0.22–0.97, P=0.04) and AP therapy (vs. AC; OR, 29.29; 95% CI, 1.36–628.93, P=0.03) were independently associated with stroke recurrence (Table 2). When age was replaced by the RoPE score, age (P=0.09) and AP therapy (P=0.61) were not significantly associated with recurrence. On the Kaplan-Meier analysis, recurrent stroke tended to be more common during AP therapy than AC therapy, although there was no significant difference (P=0.22) (Supplementary Figure 1).
We observed that AP therapy (vs. AC therapy) and low RoPE score were associated with stroke recurrence in patients with PFO-CS before PFO closure. The rate of recurrent stroke was 30 times higher with AP than with AC therapy. The high rate of stroke recurrence on AP therapy before PFO closure is a serious issue. The efficacy of AC therapy for embolic stroke of undetermined source (ESUS) has not been established. A meta-analysis of patients with ESUS and PFO found no significant difference between AC and AP therapy for ischemic stroke, although it was unclear whether the PFOs were pathogenic [8]. Another meta-analysis showed that AC therapy was more effective than AP in reducing stroke recurrence in patients with PFO and CS [6]. A stroke guideline states that, even in PFO-CS patients without VTE, AC therapy rather than AP may be considered [5]. However, direct oral anticoagulants are not covered by health insurance for patients without VTE; therefore, warfarin would be used despite the complexity of control and concerns about bleeding risk.
A low RoPE score was also independently associated with stroke recurrence. A low RoPE score (≤6 points) was associated with recurrent stroke and transient ischemic attack (TIA) [9]. In patients with low RoPE scores (≤6 points), AP (vs. AC therapy) was associated with stroke/TIA recurrence [10]. These results suggest that AP therapy is insufficient to prevent recurrence in patients with low RoPE scores before PFO closure.
Another interesting finding of our study is that 42% of patients on AP therapy had recurrent stroke. Stroke recurrence during AP therapy was considerably more common in our study than in previous reports [1-4,10]. In our study, only 2 patients without VTE had symptomatic recurrence; therefore, asymptomatic recurrence may have contributed to the high rates of stroke recurrence.
This study had some limitations. First, this was a retrospective, observational study with a small sample size. Patients were not randomized to AP and AC treatment arms. The Kaplan-Meier analysis showed no statistical difference, which may be due to small sample size, and further large-scale study is needed. Second, only patients who underwent PFO closure for preventing pathogenic PFO-CS were included. If patients not scheduled for PFO closure or with incidental PFO had been enrolled, the results may have been different. Third, magnetic resonance imaging follow-up was performed at different times by the stroke neurologists in charge.
In conclusion, recurrent stroke before PFO closure in patients with PFO-CS was more common during AP therapy and with a low RoPE score; AC therapy may be more effective than AP therapy for patients with low RoPE scores even without VTE. Further research is warranted to make our results robust.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2022.04084.
Kaplan-Meier cumulative estimates of probability of stroke in antiplatelet therapy versus anticoagulant therapy. Recurrent stroke tended to be more common during antiplatelet therapy (solid line) than anticoagulant therapy (dotted line; P=0.22).
Notes
Funding statement
This study was supported by a grant from JSPS KAKENHI (Grant Number 21K07468).
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: HK. Study design: HK. Methodology: HK. Data collection: TJ, HM, KN, MS, KO, AY, AK. Investigation: HK, TH. Statistical analysis: HK. Writing—original draft: HK. Writing—review & editing: YH, TH. Funding acquisition: HK. Approval of final manuscript: all authors.
Acknowledgements
The authors would like to express their deepest gratitude to all of the medical staff of Kyorin University Hospital.