Digital Therapeutics With Visual Discrimination Training for Cortical Blindness in Patients With Chronic Stroke
Article information
Dear Sir:
Although visual field defects (VFDs) are a devastating poststroke complication that diminishes the quality of life of stroke patients, there is no proven treatment to restore cortical blindness [1]. Recently, visual perceptual learning (VPL) with repetitive leadership training on damaged visual regions has been reported to improve visual performance [2-6]. However, evidence of the efficacy of VPL training in poststroke VFD is still lacking [5]. It is necessary to maintain central fixation during VPL training for the intervention to be effective. We devised a novel computer-based protocol that provides repetitive stimulation tasks for visual discrimination training in damaged visual fields and simultaneous ancillary stimulation tasks for central pupillary fixation to ensure appropriate training. We conducted a pilot clinical trial to explore whether this VPL protocol would be beneficial to improve VFD in chronic stroke patients. The Institutional Review Board of Asan Medical Center approved this study (IRB No. 2011-0539).
We prospectively enrolled patients with chronic stroke in the visual cortex according to the predefined criteria (Supplementary Methods). Patients who provided written informed consent were sequentially (not randomly) assigned to two groups (the VPL-trained and untrained groups) (Figure 1A). Sample size was determined to be 10 for each group in a convenient way without sample size calculation to quickly explore the performance of our protocol. For the trained group, 3 periods of VPL training were given; each period was composed of 12 training sessions (1 training session per day, 3 days per week). For the untrained group, patients did not receive VPL training. Humphrey visual field (HVF) tests (Swedish Interactive Threshold Algorithm [SITA]-Fast 30-2) were performed at baseline and at 3-month follow-up evaluations. As for the VPL protocol, we modified a previous protocol [7], which calls for dual simultaneous stimulation tasks for the training: peripheral stimulation for training and central stimulation for fixation. Peripheral stimulation was a vertical-horizontal orientation discrimination task (ODT) (“horizontal” vs. “vertical”) assigned to the defective visual field for visual training. In contrast, the central stimulation task was a distinguishing task between similar Korean letters (“ㅋ” or “ㅌ”) placed in the center (Figure 1B). VPL training location was determined on defective quadrants based on each participant’s HVF test results (Figure 1C). Visual stimuli were presented on a screen at a viewing distance of 40 cm (Figure 1D). In each trial, the ready, target, and response screens were presented sequentially (Figure 1E). While keeping their eyes fixated on the center, participants were asked to respond to dual tasks on the target screen for each trial: one to identify the fixation letter and the other to indicate the orientation of the gratings. These task stimulus types were determined randomly for each trial. After each of the 12 training sessions within a given training period, calibration was performed to adjust the stimulus contrast to the correct ratio of approximately 70% for optimizing the VPL training difficulty. Detailed protocols are provided in Supplementary Methods. Mean total deviation values were generated by averaging the scores from monocular HVFs at identical test locations between both eyes. As the main study outcome, we evaluated the HVF areas where luminance sensitivity changed by ≥6 dB to examine whether significant improvement in visual function occurred after VPL. The 6 dB cutoff value was chosen because it approximately doubles the HVF test-retest variability [8]. Areas associated with diminished visual function changes (those with sensitivity that decreased by ≥6 dB) were also analyzed as an auxiliary outcome. The Mann-Whitney U test, Wilcoxon signed-rank test, and chi-square test were each used, as appropriate, to compare the variables, including outcomes between the trained and untrained groups.
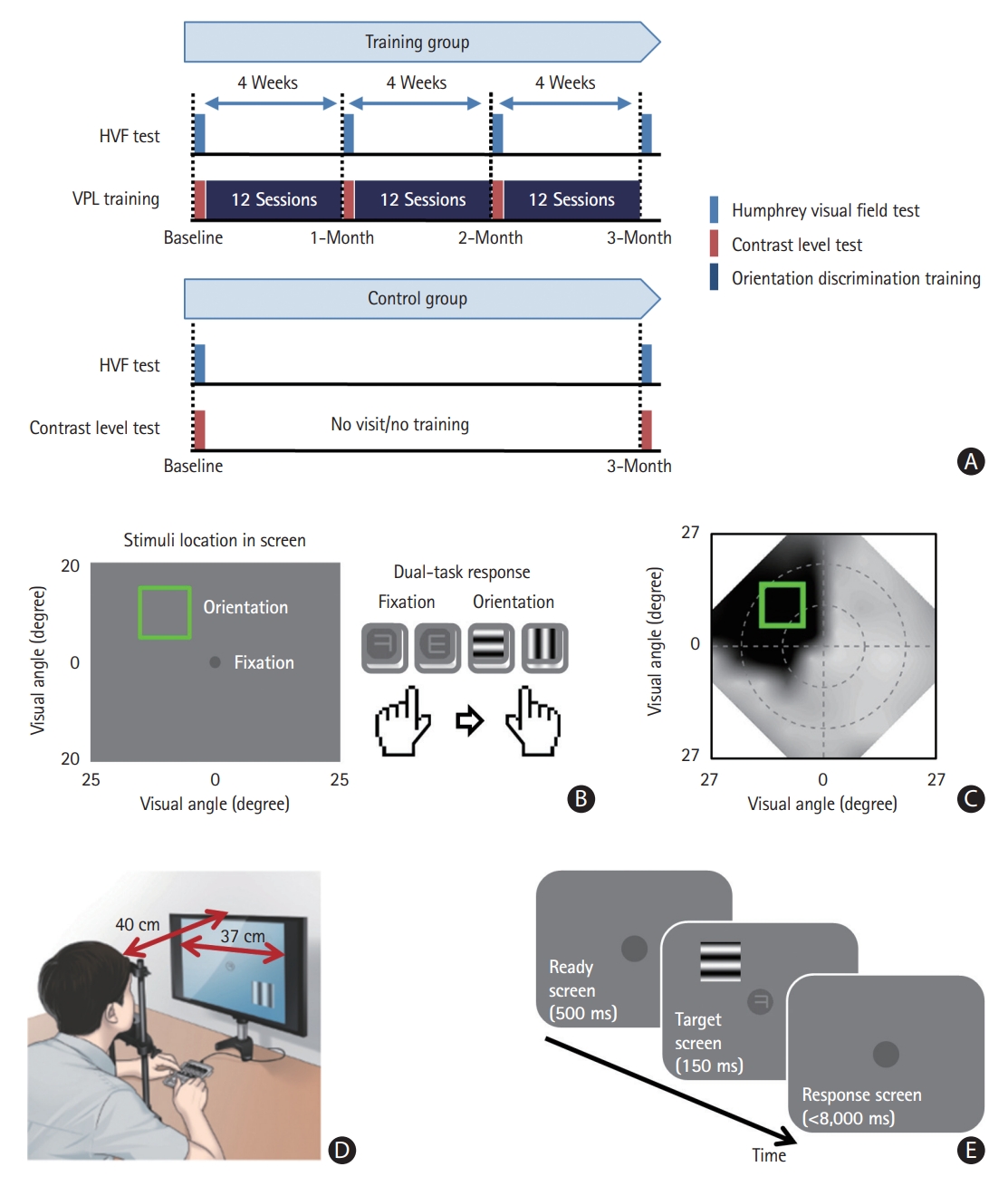
Study scheme and training protocols. (A) Study scheme. (B) Location of fixation and texture stimuli for training. A response to the fixation stimulus is required in less than 2 seconds, followed by a response to the texture stimulus within 6 seconds. The next trial starts immediately after the response to the texture stimulus. (C) An example composite Humphrey visual field test of a trained stroke patient; the green square indicates the coverage of the texture stimulus for training. (D) The training setting. (E) The trial sequence for training. HVF, Humphrey visual field; ODT, orientation discrimination task; VPL, visual perceptual learning.
Twenty patients were allocated to either the trained (n=10) or untrained (n=10) group (Table 1). The median age was 63 years; the median time between stroke onset and enrollment was 47.1 (interquartile range: 11.3 to 67.6) months. There were no significant differences in baseline variables including the degrees of baseline visual deficits (mean total deviation) between the treatment groups. All patients in the trained group successfully underwent the training protocol without dropping out. We evaluated whether visual function improved with VPL training. After 3 months, areas with improved visual function were significantly larger in the trained group than in the untrained group (median [interquartile ranges]: 288 [216–648] vs. 72 [36–180] degree [2], P=0.004) (Figure 2A). Meanwhile, the sizes of the areas with diminished visual function were comparable (Figure 2B). The luminance sensitivity, measured by mean total deviation values, was significantly improved only in the trained group (Figure 2C). Accordingly, changes in mean total deviation were also significantly greater in the trained group than in the untrained group (2.1 [0.3–5.2] vs. 0.0 [-0.6–0.5], P=0.011) (Figure 2D).
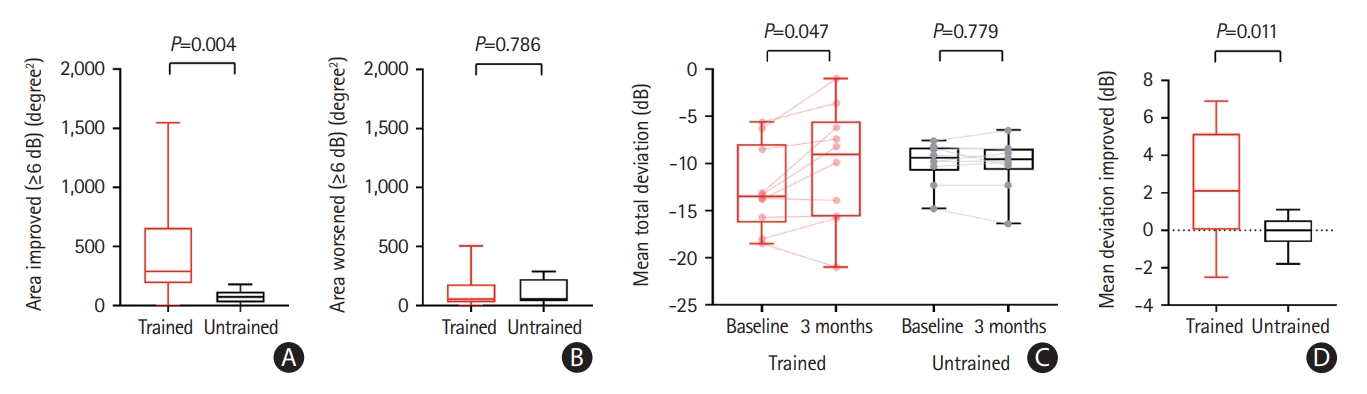
Outcome variables between the untrained and trained groups. (A) Areas improved (≥6 dB); (B) areas worsened (≥6 dB); (C) changes in mean total deviation (dB) between baseline and 3 months; (D) mean total deviation improved between baseline and 3 months.
There are several remarkable points. First, the VPL protocol in this study uses simultaneous presentation of central fixation stimuli and ODT stimuli. Central fixation is a prerequisite to inducing effective VPL, enabling sufficient visual stimulation to damaged visual fields. Second, the degree of improved visual function is significant and clinically meaningful. The median degree of improved area in the trained group was 288 degree [2]. This corresponds to 8 points on the HVF test, which is much higher than the 3 HVF test point (108 degree [2]) cutoff to determine significant visual deterioration for patients with glaucoma [9]. Third, our computer-based VPL protocol has the potential to be used in digital therapeutics. Digital tools have strengths in that they could provide patient-specific training stimuli by flexibly changing training protocols [10]. Meanwhile, the limitations that are inherent to a pilot study should also be noted, such as the small sample size and the lack of randomization with a small proportion of female patients. Additionally, the study had a short follow-up period, and long-term visual function outcomes were not evaluated. A lack of investigation of the neural mechanisms underlying VPL is another limitation.
Nevertheless, our novel VPL training protocol with dual tasks for peripheral ODT and central fixation was feasible and significantly improved visual function in chronic stroke patients with VFDs. These findings suggest the potential effectiveness of digital therapeutics with VPL training in patients with cortical blindness, which warrants future studies.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2023.00276.
Notes
Funding statement
This research was supported by a grant from the Korea Health Technology R&D Project, through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare (HR18C0016), a grant from National IT Industry Promotion Agency (NIPA) funded by the Korea government (MSIT) (No. S0252-21-1001, Development of AI Precision medical Solution [Doctor Answer2.0]), a grant from National Research Foundation of Korea (NRF) funded by the Korea government (MSIT) (2022R1F1A1060778), Republic of Korea, and grants from NIH (EY031705, R01 EY027841, R01 EY019466), USA.
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: DK, DWK. Study design: DWK. Methodology: DK, DWK. Data collection: JHL, DK, YHK. Investigation: JHL, YHK. Statistical analysis: EJL, YHK, EN. Writing—original draft: EJL, DK, DWK. Writing—review & editing: all authors. Funding acquisition: DWK, EN, YS, TW. Approval of final manuscript: all authors.

