Association of Coronary Stenosis With Cerebral Small Vessel Diseases in Neurologically Asymptomatic Adults
Article information
Dear Sir:
Stroke and ischemic heart disease usually cause sudden death or disabilities. Therefore, early identification and risk management for high-risk groups are important. Cerebral small vessel diseases (cSVD) are known to lead to diseases such as stroke and dementia [1], and asymptomatic coronary artery stenosis (CAS) is considered a subclinical condition of ischemic heart disease. Previous studies have demonstrated associations between stroke and asymptomatic CAS [2] and between cSVD and ischemic heart disease [3]. However, to our best knowledge, no studies have investigated the association between asymptomatic CAS and subclinical cSVD in screening populations. We aimed to evaluate this potential association by analyzing brain magnetic resonance imaging (MRI) and coronary computed tomography angiography (CCTA) data from an asymptomatic screening population.
We used a health check-up registry from the Seoul National University Hospital Health Promotion Center between January 2010 and December 2013. We retrospectively evaluated 1,627 participants who underwent voluntary screening health check-ups, including both brain MRI and concomitant CCTA. We excluded participants with a history of previous stroke, myocardial infarction, or angina (n=56). Finally, 1,571 participants who were neurologically and cardiologically asymptomatic were enrolled. This study was approved by the Institutional Review Board of the Seoul National University Hospital (approval number: 1502-026-647), and the requirement of informed consent was waived. All experiments were performed in accordance with the Declaration of Helsinki and relevant guidelines and regulations.
The presence of CAS was evaluated semiquantitatively and described as the greatest percentage of the lumen diameter reduction among the three epicardial coronary arteries, including the left anterior descending artery, left circumflex artery, and right coronary artery, estimated as multiples of 5% [4]. If stenosis was noted in two or more coronary arteries, the value with the highest degree of stenosis was selected. We classified CAS into three groups, no stenosis (0%), non-significant stenosis (1%–49%), and significant stenosis (≥50%).
We evaluated all three components of cSVD, including lacunes, cerebral microbleeds (CMBs), and white matter hyperintensity (WMH). A lacune was defined as a focal infarction, measuring 3–15 mm, in the territory of the perforating branches to the basal ganglia, thalamus, internal capsule, corona radiata, centrum semiovale, brain stem, or cerebellum, with a central signal intensity corresponding to the cerebrospinal fluid on T1- and T2-weighted images in MRI examinations [5]. A CMB was defined as a focal round lesion, measuring <10 mm, with a low signal on T2-gradient echo images [6], and the WMH volume was measured using a computer-assisted semiautomated technique (Medical Image Processing, Analysis, and Visualization [MIPAV] version 7.3.0; National Institutes of Health, Bethesda, MD, USA). We transformed the WMH volume into a square root scale because of the excessive number of zeroes [7]. We also collected clinical variables including cardiovascular risk factors. Details of the measurements and definitions are provided in the Supplementary Methods.
To assess the relationship between CAS and cSVD, we performed logistic regression analyses for the presence of lacunes and CMBs and linear regression analysis for WHM volume. In the multivariate analyses, we included age, sex, body mass index (BMI), smoking status, exercise, hypertension, diabetes mellitus (DM), and dyslipidemia as confounders because they are well-established cardiovascular risk factors [8]. According to previous studies, alcohol consumption was assumed to be a possible confounder [4]. Additionally, waist circumference (WC) and estimated glomerular filtration rate (eGFR) were considered possible confounders because significant associations were observed in the univariate analyses. Therefore, multivariate analyses were adjusted for age, sex, BMI, WC, smoking and alcohol consumption status, exercise, hypertension, DM, dyslipidemia, and eGFR.
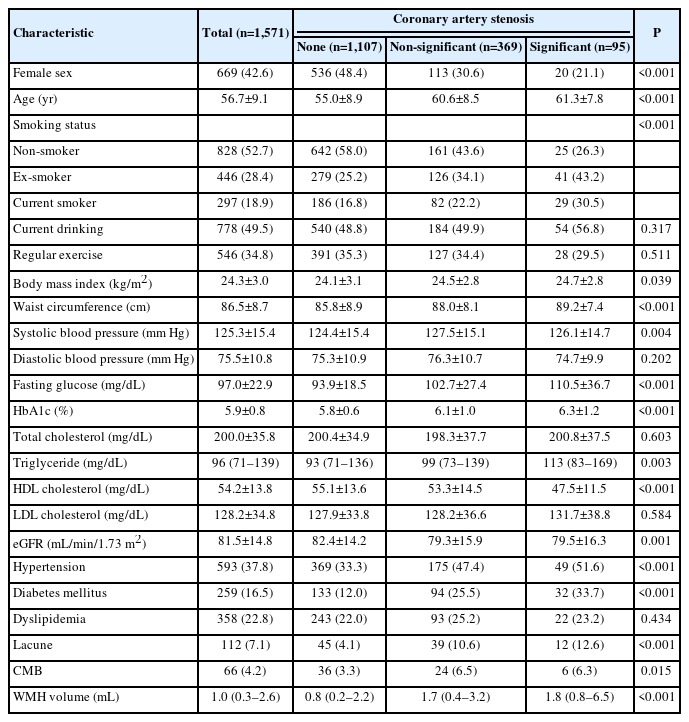
We included 1,571 neurologically and cardiologically asymptomatic participants (mean age, 56.7 years; female, 42.6%). Non-significant and significant CAS were observed in 369 (23.5%) and 95 (6.1%) participants, respectively. The prevalence of lacunes and CMBs was 112 (7.1%) and 66 (4.2%), respectively. The median WMH volume was 1.0 (interquartile range, 0.3–2.6) mL. Regarding the smoking status, 828 (52.7%) participants were non-smokers, 446 (28.4%) were ex-smokers, and 297 (18.9%) were current smokers. In total, 593 (37.8%) participants had hypertension, 259 (16.5%) had DM, and 358 (22.8%) had dyslipidemia. The other detailed baseline characteristics of the study participants are presented in Table 1.
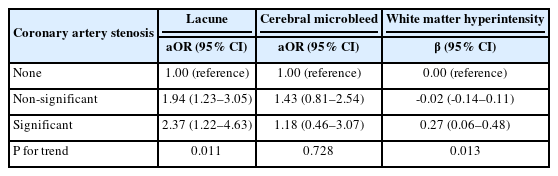
Non-significant CAS (adjusted odds ratio [aOR]=1.94, 95% confidence interval [CI]=1.23–3.05) and significant CAS (aOR=2.37, 95% CI=1.22–4.63) were significantly associated with lacunes after adjusting for possible confounders (Table 2). CAS severity was associated with an increasing trend in the prevalence of lacunes (P for trend=0.011). For CMBs, no statistical significance was observed. For WMH, only significant CAS (β=0.27, 95% CI= 0.06–0.48) showed a statistically significant association. These parameters also showed dose–response relationships (P for trend=0.013) (Table 2).
Considering that hypertension is the strongest modifiable risk factor for cSVD, we performed stratified analyses based on the hypertension status. For CMB, a significant association appeared in hypertensive groups (none vs. non-significant CAS, aOR=2.48, 95% CI=1.15–5.32) (Table 3). In addition, consistent results were obtained in the sensitivity analyses of the population without intracranial/extracranial stenosis or without receiving antithrombotic agents (Supplementary Table 1).

Multivariate analyses comparing coronary artery stenosis and cerebral small vessel diseases stratified by hypertension status
This study revealed significant associations between CAS and both lacunes and WMH. For CMBs, a significant association was observed only in the hypertensive group. These results can be partly explained by the following mechanisms. First, endothelial dysfunction can cause blood–brain barrier breakdown, resulting in perivascular tissue and arteriolar wall damage, factors important for CAS and lacunes/WMH [1]. Second, oxidative stress resulting in chronic inflammation can lead to CAS and lacunes/WMH. Various noxious stimuli that induce vascular oxidative stress have been implicated in the pathogenesis of various disease states, including coronary artery disease [9] and stroke [10]. CMBs are generally considered to originate from hypertensive vasculopathy or cerebral amyloid angiopathy. The strong contribution of hypertension to both CAS and CMB development might explain their positive association in hypertensive individuals.
In conclusion, we investigated the association between CAS and cSVD in neurologically and cardiologically asymptomatic adults and found a positive association between them. Therefore, physicians who detect CAS or cSVD must pay attention to the possible coexistence of the other disease and consider screening tests for early detection and management.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2023.01732.
Multivariate analyses comparing coronary artery stenosis and cerebral small vessel diseases in the sensitivity analyses
Notes
Funding statement
None
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: HMK, JHP. Study design: KM, JMY, SEH, JHP. Methodology: KWN, HYJ, HMK. Data collection: KM, JMY, SEH, JHP. Investigation: KM, JMY, SEH, JHP. Statistical analysis: JMY. Writing—original draft: KM, JMY. Writing—review & editing: HMK, JHP. Approval of final manuscript: all authors.