 |
 |
- Search
| J Stroke > Volume 26(1); 2024 > Article |
|
Abstract
Background and Purpose
Outcomes following mechanical thrombectomy (MT) are strongly correlated with successful recanalization, traditionally defined as modified Thrombolysis in Cerebral Infarction (mTICI) ≥2b. This retrospective cohort study aimed to compare the outcomes of patients with low Alberta Stroke Program Early Computed Tomography Score (ASPECTS; 2-5) who achieved mTICI 2b versus those who achieved mTICI 2c/3 after MT.
Methods
This study utilized data from the Stroke Thrombectomy and Aneurysm Registry (STAR), which combined databases from 32 thrombectomy-capable stroke centers between 2013 and 2023. The study included only patients with low ASPECTS who achieved mTICI 2b, 2c, or 3 after MT for internal carotid artery or middle cerebral artery (M1) stroke.
Results
Of the 10,229 patients who underwent MT, 234 met the inclusion criteria. Of those, 98 (41.9%) achieved mTICI 2b, and 136 (58.1%) achieved mTICI 2c/3. There were no significant differences in baseline characteristics between the two groups. The 90-day favorable outcome (modified Rankin Scale score: 0-3) was significantly better in the mTICI 2c/3 group than in the mTICI 2b group (adjusted odds ratio 2.35; 95% confidence interval [CI] 1.18-4.81; P=0.02). Binomial logistic regression revealed that achieving mTICI 2c/3 was significantly associated with higher odds of a favorable 90-day outcome (odds ratio 2.14; 95% CI 1.07-4.41; P=0.04).
The current endpoint for successful endovascular treatment of large vessel occlusion (LVO) of the anterior circulation is achievement of a modified Thrombolysis in Cerebral Ischemia (mTICI) score of 2b or greater as multiple studies have demonstrated a strong association with this angiographic, recanalization outcome and subsequent neurologic and clinical recovery [1-3]. Furthermore, recent reports have assessed the outcomes of angiographic mTICI scores greater than 2b and have demonstrated a continuous relationship between recanalization grade and functional outcome [4]. As the number of mechanical thrombectomy (MT) attempts has been revealed to have a negative correlation with patient outcomes, operators are faced with balancing maximizing angiographic recanalization grade with thrombectomy retrieval attempts [5-9].
Patients with LVO of the anterior circulation with a low Alberta Stroke Program Early Computed Tomography Score (ASPECTS) of less than 6 were previously thought to not be ideal candidates for MT due to relatively smaller volume of salvageable penumbra and risk of cerebral hemorrhage. Recent randomized clinical trials have demonstrated that this patient population may attain long term functional independence after MT if they achieve successful recanalization defined as a recanalization grade of 2b or greater [10,11]. However, the presence of a similar continuous relationship between recanalization grade and functional outcome, as previously demonstrated for patients with ASPECTS 6-10, has yet to be demonstrated among low ASPECTS patients. Among a large, real-world population of patients undergoing MT with low ASPECTS (2-5) on presentation, we investigated whether achieving mTICI 2c/3 recanalization confers additional benefit for outcome compared to mTICI 2b.
This cohort study utilized data from the Stroke Thrombectomy and Aneurysm Registry (STAR), a prospectively maintained retrospective database comprising 32 thrombectomy-capable stroke centers in the US, Europe, and Asia. Ethical approval was obtained from the institutional review board (IRB) at each participating center, and data analysis was conducted at the core institution. The requirement of informed consent was waived by IRBs. Each center autonomously collected comprehensive data, including basic demographic characteristics, medical history, comorbidities, admission National Institutes of Health Stroke Scale (NIHSS) score, occluded vessels, ASPECTS, time from symptom onset to groin puncture, procedure time, devices utilized, final mTICI score, functional outcomes (evaluated using modified Rankin Scale [mRS]), and complications.
We included all patients who underwent MT for internal carotid artery (ICA) or M1 segment of middle cerebral artery occlusions and achieved mTICI of 2b or more up until May 30, 2023. Patients were stratified into mTICI 2b and mTICI 2c/3 groups. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement criteria [12].
The primary outcome was favorable clinical outcome at 90 days, defined as a 90-day mRS score of 0-3. The mRS score was assessed during follow-up visits or telephone encounters at 90±30 days. Additional outcomes included mRS scores of 0-2, mortality at 90 days, successful recanalization, any hemorrhage, and symptomatic intracranial hemorrhage (sICH). Successful recanalization was defined as mTICI 2b or higher [13,14]. sICH was defined as intracranial hemorrhage with an associated worsening of 4 points or more in the NIHSS score at 24 hours post-procedure [15]. Neurological improvement defined as 4 points improvement on the NIHSS [16,17].
All statistical analyses were performed using R (version 4.2.2; R Foundation for Statistical Computing, Vienna, Austria). Continuous variables were presented as median (interquartile range [IQR]), while categorical variables were reported as percentages. Between-group comparisons of characteristics were conducted using the Wilcoxon rank-sum (Mann-Whitney) test and the χ2 test, as appropriate. We employed a binomial multivariate logistic regression model to assess factors associated with 90-day favorable outcomes in all patients undergoing MT with ICA or M1 occlusion. The variables included in the regression model were age, sex, ICA occlusion, ASPECTS, admission NIHSS score, intravenous thrombolysis, mTICI 2c/3, time from symptom onset to groin puncture, and procedure duration. All P-values were derived from 2-sided tests, and statistical significance was set at P<0.05.
Of the 10,229 consecutive patients who underwent thrombectomy, 234 met the inclusion criteria. Among the included subset, 136 (58.1%) achieved an mTICI of 2c/3 and 98 (41.9%) achieved an mTICI of 2b (Figure 1).
Table 1 summarizes the baseline, clinical, and procedural characteristics of patients in the mTICI 2b and mTICI 2c/3 groups. There were no significant differences in age, sex, comorbidities, admission NIHSS, ASPECTS, and use of intravenous thrombolysis between the two groups (P>0.05). However, the distribution of occluded vessels differed significantly between the mTICI 2b and mTICI 2c/3 groups (P<0.01). M1 occlusion was observed in 37.8% of cases in the mTICI 2b group compared to 58.1% in the mTICI 2c/3 group. ICA occlusion was present in 37.8% of cases in the mTICI 2b group compared to 27.9% in the mTICI 2c/3 group. Both M1 and ICA occlusion were observed in 24.5% of cases in the mTICI 2b group compared to 14.0% in the mTICI 2c/3 group.
Patients who achieved mTICI 2b required a higher number of procedural attempts, with a median of 3 attempts (IQR 2-4), compared to a median of 2 attempts (IQR 1-3) in the mTICI 2c/3 group (P<0.01). The procedure duration was longer for patients in the mTICI 2b group, with a median of 53 minutes (IQR 28-80), compared to a median of 29 minutes (IQR 15-59) in the mTICI 2c/3 group (P<0.01).
The mTICI 2c/3 group demonstrated a significantly higher rate of favorable outcomes at 90 days, defined as mRS score of 0-3, compared to the mTICI 2b group (adjusted odds ratio [aOR]=2.35; 95% confidence interval [CI]=1.18-4.81; P=0.02). There was no significant difference between the two groups in achieving functional independence (mRS 0-2) (aOR=1.78; 95% CI=0.77-4.31; P=0.20). The proportion of patients with an mRS score of 0-3 at 90 days was significantly higher in the mTICI 2c/3 group, with 60 patients (44.1%), compared to 24 patients (24.5%) in the mTICI 2b group (P<0.01). The distribution of mRS scores among the mTICI 2b and mTICI 2c/3 groups is depicted in Figure 2. mTICI 2c/3 group showed significantly higher neurological improvement at 24 hours post-procedure and at discharge (aOR 2.01, 95% CI=1.04-4.28; P=0.04; aOR=2.76; 95% CI=1.31-6.01; P<0.01, respectively).
Both sICH and mortality rates were no different between the mTICI 2c/3 and mTICI 2b groups (sICH: aOR=1.30, 95% CI=0.58-3.04, P=0.60; mortality: aOR=0.68, 95% CI=0.38-1.24, P=0.20, respectively). However, distal embolization was significantly higher in the mTICI 2b group (aOR=0.16; 95% CI=0.07-0.34; P<0.01) (Table 2).
Further comparison of mTICI 2c (n=33) recanalization with mTICI 3 (n=103) showed no significant difference between the two groups in terms of clinical outcomes and complications (Table 3).
A binary logistic regression analysis was conducted to identify predictors of 90-day outcome in low ASPECTS stroke patients who underwent MT for ICA or M1 occlusion. The analysis revealed that younger age (OR, 0.95; 95% CI, 0.92-0.97; P<0.01), lower admission NIHSS score (OR, 0.91; 95% CI, 0.86-0.96; P<0.01), and mTICI score of 2c/3 (OR, 2.14; 95% CI, 1.07-4.41; P=0.04) were significantly associated with favorable 90-day outcomes (mRS 0-3). However, no significant associations were found for procedure duration, time from symptom onset to groin puncture, female sex, intravenous thrombolysis, ICA occlusion, and ASPECTS (Table 4).
This large, multicenter, real-world experience series investigates the clinical outcomes of patients with acute LVO and low ASPECTS on presentation treated with MT and achieving a post-thrombectomy recanalization grade of mTICI 2b versus 2c/3. We found that a recanalization grade of mTICI 2c/3 was associated with a significantly higher rate of achieving a good functional outcome of mRS of 0-3 at 90 days compared to mTICI 2b. Moreover, despite the theoretical increased risk of recanalization-associated hemorrhagic transformation occurring in patients with large core infarcts undergoing successful thrombectomy, the rates of hemorrhage were not observed to be different between the two cohorts.
Recently published randomized controlled trials [18-20] and large multicenter registry data [10,11,21-25] have provided definitive evidence for beneficial effect of MT in LVO patients with low ASPECTS. In a large, multicenter, retrospective series, Almallouhi et al. [10] demonstrated that more than 1 in 5 patients presenting with an ASPECTS of 2 to 5 achieved 90-day functional independence after MT, and a favorable outcome was nearly five times more likely for patients with low ASPECTS who had successful recanalization. This functional recovery was similarly found in patients presenting in both the early and extended windows. Altogether, current evidence demonstrates that patients with low ASPECTS can have a good functional recovery following successful thrombectomy.
Beyond mTICI 2b, the additional positive impact on outcome for achieving mTICI 2c/3 among small core patients has been emphasized in the literature and has led practitioners to strive to maximize the post-thrombectomy recanalization grade. Early recommendations considered achieving mTICI of 2b or higher to be a successful recanalization and did not necessarily recommend increasing the number of thrombectomy attempts to achieve an mTICI 2c/3 if a grade of 2b had already been achieved [1,3]. However, a recently published meta-analysis identified an incremental association between mTICI score and clinical outcome, emphasizing the importance of maximizing recanalization grade to greater than 2b if possible [26]. More recent data from a large multicenter registry further confirmed this notion and reported a positive, continuous relationship between recanalization grade and functional outcomes, with an extended thrombolysis in cerebral infarction of 3 leading to the best outcome [4]. In our study, we found similar degree of benefit of mTICI 2c/3 compared to mTICI 2b in patients with low ASPECTS. Whether additional passes or adjunct therapy such as intra-arterial thrombolysis should be considered to achieve complete recanalization is yet to be answered.
The role of thrombectomy attempts on procedural complications and outcome has been thoroughly assessed and reported in the literature. Several studies have demonstrated a negative impact on outcomes following multiple thrombectomy attempts with best outcomes occurring in patients requiring only one attempt [5-8,22,27,28]. Even among patients with failed recanalization (mTICI 0), more than two attempts were associated with a worse clinical outcome, demonstrating the harmful effect of multiple thrombectomy attempts [8]. Ultimately, neurointerventionalists are left with the goal of optimizing post-thrombectomy recanalization grade with as minimal amount of attempts as possible, with the knowledge that greater than two attempts has a potentially harmful effect on patient outcomes, but also knowing that successful recanalization is the only chance the patient has to restore neurologic function.
In the setting of patients with LVO and low ASPECT that undergo thrombectomy, the clinical significance of an mTICI grade of 2b versus 2c/3 is not well defined, and the role of balancing thrombectomy attempts to achieve a maximal recanalization grade as demonstrated by previous data in cohorts of patients with high mTICI grades, may not apply to patients with low ASPECT. This study demonstrates that patients with an ASPECT of 2-5 that achieved a recanalization grade of mTICI 2c/3 had a significantly higher rate of achieving a good functional outcome of mRS of 0-3 at 90 days compared to the mTICI 2b cohort. Furthermore, a subgroup analysis demonstrated that this clinical significance was not maintained when comparing the mTICI 2c cohort to mTICI 3.
While these two cohorts were well matched, as shown by the comparable baseline characteristics, there were interesting periprocedural differences that are worth noting. Primarily, the median number of thrombectomy attempts seen on the mTICI 2b cohort of 3 was significantly higher than the mTICI 2c/3 cohort of 2. Additionally, the procedural duration was significantly higher in the mTICI 2b. This increase in attempts observed could be a consequence of a more complex pathology or anatomy present in the mTICI 2b group that was not accounted for in this analysis that is impacting the difference in number of thrombectomy attempts and functional outcome. This undefined variable could also be the driver of the difference seen in procedural duration time. Nonetheless, even after adjusting for age and location of occlusion, the mTICI 2c/3 group still demonstrated better functional outcomes.
Importantly, the rates of both any intracerebral hemorrhage and sICH were similar between the two cohorts. Given the higher rates of post-thrombectomy intracerebral hemorrhage associated with successful recanalization in patients with low ASPECTS compared to patients with high ASPECTS, it was important to determine whether a higher mTICI grade similarly was associated with a higher rate of hemorrhage in patients with low ASPECTS. This study provides evidence that an mTICI of 2c/3 is associated with improved functional outcome at 90 days without any associated difference in post-thrombectomy intracerebral hemorrhage.
There are several limitations in this study that must be noted. Primarily, as this is a retrospective, observational study, causality cannot be concluded, and further randomized control trials must be performed to further assess the role of mTICI score on patient outcomes. Additionally, as this is a multicenter study, there is likely heterogeneity in the periprocedural management of the patients in this study. Moreover, as the ASPECTS and mTICI scores were calculated by the investigators at the sites included in this study, there may be interrater variance. Lastly, this study did not include data regarding diffusion imaging. Future studies will benefit from both interrater reliability protocols and incorporation of perfusion and diffusion imaging data.
This large multicenter study provides evidence that the degree of successful recanalization in patients with low ASPECTS on presentation that undergo thrombectomy for LVO of the anterior circulation correlates with 90-day good functional outcome. A recanalization grade of mTICI 2c/3 resulted in greater likelihood of good outcome compared to mTICI 2b, without a trade-off of higher rates post-procedure hemorrhage. While further studies are necessary to validate these findings, it is recommended that a post-thrombectomy recanalization grade mTICI grade of 2c/3 is recommended in patients with low ASPECTS.
Notes
Conflicts of interest
The disclosures of conflicts of interest of all authors are provided in Appendix 1.
Author contribution
Conceptualization: SSE, AMS, SA. Study design: SSE, BFS, HM, KU, AMS, SA. Methodology: SSE, BFS, HM, KU, AMS, SA. Data collection: all authors. Investigation: all authors. Statistical analysis: SSE, HM, KU, AMS, SA. Writing—original draft: SSE, BFS, AMS, SA. Writing—review & editing: all authors. Funding acquisition: AMS. Approval of final manuscript: all authors.
Acknowledgments
We would like to thank all investigators for their efforts in conducting the Stroke Thrombectomy and Aneurysm Registry (STAR) Collaborators.
Figure 1.
Patient selection flow chart. STAR, Stroke Thrombectomy and Aneurysm Registry; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; M1, M1 segment of the middle cerebral artery; ICA, internal carotid artery; mTICI, modified Thrombolysis in Cerebral Infarction; mRS, modified Rankin Scale.
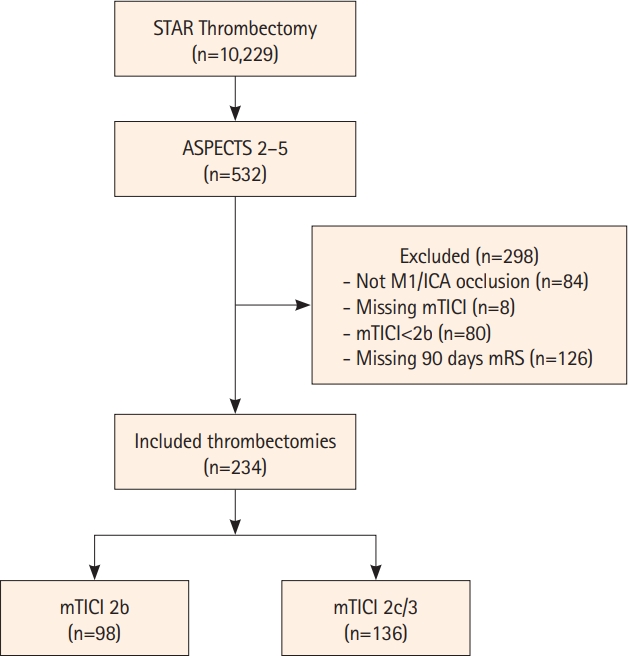
Figure 2.
Scores on the mRS at 90 days for low ASPECTS patients who underwent mechanical thrombectomy for internal carotid artery or M1 occlusion with achievement of recanalization grade of mTICI 2b versus 2c/3. mRS, modified Rankin Scale; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; M1, middle cerebral artery; mTICI, modified Thrombolysis in Cerebral Infarction.
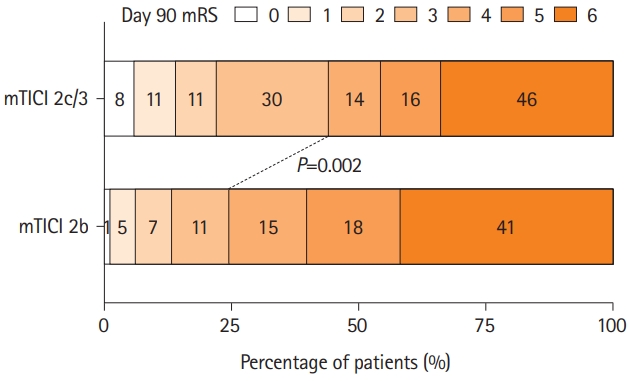
Table 1.
Characteristics of low ASPECTS patients who underwent mechanical thrombectomy for ICA or M1 occlusion with achievement of recanalization grade of mTICI 2b or 2c/3
Data are expressed as median [interquartile range] or number of cases (%).
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; ICA, internal carotid artery; M1, middle cerebral artery; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institutes of Health Stroke Scale; IV-tPA, intravenous tissue plasminogen activator; CTA, computed tomography angiography; CTP, computed tomography perfusion; DWI, diffusion-weighted imaging; ADAPT, A Direct Aspiration first Pass Technique; IAtPA, intra-arterial tissue plasminogen activator.
Table 2.
Outcomes of low ASPECTS patients who underwent mechanical thrombectomy for ICA or M1 occlusion with achievement of recanalization grade of mTICI 2b versus 2c/3
| Outcome | mTICI 2c/3 (n=136) | mTICI 2b (n=98) | Crude OR (95% CI) | P | Adjusted OR* (95% CI) | P |
|---|---|---|---|---|---|---|
| mRS 0-3 | 60 (44.1) | 24 (24.5) | 2.43 (1.39-4.37) | <0.01 | 2.35 (1.18-4.81) | 0.02 |
| mRS 0-2 | 30 (22.1) | 13 (13.3) | 1.85 (0.93-3.88) | 0.09 | 1.78 (0.77-4.31) | 0.20 |
| Neurological improvement at 24 hours† | 59 (55.7) | 23 (34.8) | 2.35 (1.25-4.48) | <0.01 | 2.01 (1.04-4.28) | 0.04 |
| Neurological improvement at discharge† | 65 (62.5) | 29 (43.3) | 2.18 (1.17-4.11) | 0.01 | 2.76 (1.31-6.01) | <0.01 |
| Symptomatic intracranial hemorrhage | 20 (14.7) | 13 (13.5) | 1.10 (0.52-2.39) | 0.80 | 1.30 (0.58-3.04) | 0.60 |
| Any hemorrhage | 55 (40.7) | 37 (38.5) | 1.10 (0.64-1.88) | 0.70 | 1.03 (0.57-1.85) | 0.70 |
| Distal embolization | 15 (11.3) | 35 (38.0) | 0.21 (0.10-0.40) | <0.01 | 0.16 (0.07-0.34) | <0.01 |
| 90-Day mortality | 46 (33.8) | 41 (41.8) | 0.71 (0.42-1.22) | 0.20 | 0.68 (0.38-1.24) | 0.20 |
Data were expressed as number of cases (%), unless otherwise indicated.
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; ICA, internal carotid artery; M1, middle cerebral artery; mTICI, modified Thrombolysis in Cerebral Infarction; OR, odds ratio; CI, confidence interval; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; IV-tPA, intravenous tissue plasminogen activator.
Table 3.
Outcomes of low ASPECTS patients who underwent mechanical thrombectomy for ICA or M1 occlusion with achievement of recanalization grade of mTICI 2c versus 3
| Outcome | mTICI 3 (n=103) | mTICI 2c (n=33) | Crude OR (95% CI) | P | Adjusted OR* (95% CI) | P |
|---|---|---|---|---|---|---|
| mRS 0-3 | 43 (41.7) | 17 (51.5) | 0.67 (0.30-1.48) | 0.30 | 1.01 (0.34-3.10) | >0.99 |
| mRS 0-2 | 22 (21.4) | 8 (24.2) | 0.85 (0.35-2.24) | 0.70 | 0.84 (0.24-3.25) | 0.80 |
| Neurological improvement at 24 hours† | 43 (54.4) | 16 (59.3) | 0.82 (0.33-1.98) | 0.70 | 1.03 (0.34-3.14) | >0.99 |
| Neurological improvement at discharge† | 48 (59.3) | 17 (73.9) | 0.51 (0.17-1.38) | 0.20 | 0.39 (0.07-1.63) | 0.20 |
| Any hemorrhage | 38 (37.3) | 17 (51.5) | 0.56 (0.25-1.23) | 0.15 | 0.46 (0.16-1.24) | 0.13 |
| Symptomatic intracranial hemorrhage | 13 (12.6) | 7 (21.2) | 0.54 (0.20-1.55) | 0.20 | 0.36 (0.11-1.15) | 0.08 |
| 90-Day mortality | 37 (35.9) | 9 (27.3) | 1.49 (0.65-3.71) | 0.40 | 0.74 (0.24-2.28) | 0.60 |
Data were expressed as number of cases (%), unless otherwise indicated.
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; ICA, internal carotid artery; M1, middle cerebral artery; mTICI, modified Thrombolysis in Cerebral Infarction; OR, odds ratio; CI, confidence interval; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; IV-tPA, intravenous tissue plasminogen activator.
Table 4.
Multivariate regression analysis for predictors of 90-day mRS 0-3
mRS, modified Rankin Scale; OR, odds ratio; CI, confidence interval; NIHSS, National Institutes of Health Stroke Scale; mTICI, modified Thrombolysis in Cerebral Infarction; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; IV-tPA, intravenous tissue plasminogen activator; ICA, internal carotid artery.
References
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019;50:e344-e418.

2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018;49:e46-e110.

3. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 2019;11:535-538.


4. LeCouffe NE, Kappelhof M, Treurniet KM, Lingsma HF, Zhang G, van den Wijngaard IR, et al. 2B, 2C, or 3: what should be the angiographic target for endovascular treatment in ischemic stroke? Stroke 2020;51:1790-1796.


5. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke 2018;49:660-666.


6. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke 2019;50:2140-2146.


7. Flottmann F, Brekenfeld C, Broocks G, Leischner H, McDonough R, Faizy TD, et al. Good clinical outcome decreases with number of retrieval attempts in stroke thrombectomy: beyond the first-pass effect. Stroke 2021;52:482-490.


8. Flottmann F, van Horn N, Maros ME, Leischner H, Bechstein M, Meyer L, et al. More retrieval attempts are associated with poorer functional outcome after unsuccessful thrombectomy. Clin Neuroradiol 2022;32:361-368.




9. Alawieh A, Vargas J, Fargen KM, Langley EF, Starke RM, De Leacy R, et al. Impact of procedure time on outcomes of thrombectomy for stroke. J Am Coll Cardiol 2019;73:879-890.


10. Almallouhi E, Al Kasab S, Hubbard Z, Bass EC, Porto G, Alawieh A, et al. Outcomes of mechanical thrombectomy for patients with stroke presenting with low Alberta Stroke Program Early Computed Tomography Score in the early and extended window. JAMA Netw Open 2021;4:e2137708.


11. Hungerford JP, Hyer M, Turk AS, Turner RD, Chaudry MI, Fargen KM, et al. Impact of ASPECT scores and infarct distribution on outcomes among patients undergoing thrombectomy for acute ischemic stroke with the ADAPT technique. J Neurointerv Surg 2017;9:823-829.


12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-1457.


13. Manning NW, Chapot R, Meyers PM. Endovascular stroke management: key elements of success. Cerebrovasc Dis 2016;42:170-177.



14. Badhiwala JH, Nassiri F, Alhazzani W, Selim MH, Farrokhyar F, Spears J, et al. Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA 2015;314:1832-1843.


15. Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA 1995;274:1017-1025.


16. Haley EC Jr, Levy DE, Brott TG, Sheppard GL, Wong MC, Kongable GL, et al. Urgent therapy for stroke. Part II. Pilot study of tissue plasminogen activator administered 91-180 minutes from onset. Stroke 1992;23:641-645.


17. Brott TG, Haley EC Jr, Levy DE, Barsan W, Broderick J, Sheppard GL, et al. Urgent therapy for stroke. Part I. Pilot study of tissue plasminogen activator administered within 90 minutes. Stroke 1992;23:632-640.


18. Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med 2023;388:1272-1283.

19. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 2022;386:1303-1313.


20. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med 2023;388:1259-1271.

21. Campbell BCV, Majoie CBLM, Albers GW, Menon BK, Yassi N, Sharma G, et al. Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy: a meta-analysis of individual patient-level data. Lancet Neurol 2019;18:46-55.

22. Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol 2018;17:895-904.

23. Mourand I, Abergel E, Mantilla D, Ayrignac X, Sacagiu T, Eker OF, et al. Favorable revascularization therapy in patients with ASPECTS ≤ 5 on DWI in anterior circulation stroke. J Neurointerv Surg 2018;10:5-9.


24. Kaesmacher J, Chaloulos-Iakovidis P, Panos L, Mordasini P, Michel P, Hajdu SD, et al. Mechanical thrombectomy in ischemic stroke patients With Alberta Stroke Program Early Computed Tomography Score 0-5. Stroke 2019;50:880-888.


25. Cagnazzo F, Derraz I, Dargazanli C, Lefevre PH, Gascou G, Riquelme C, et al. Mechanical thrombectomy in patients with acute ischemic stroke and ASPECTS ≤6: a meta-analysis. J Neurointerv Surg 2020;12:350-355.


26. Yoo AJ, Berkhemer OA, Fransen PSS, van den Berg LA, Beumer D, Lingsma HF, et al. Effect of baseline Alberta Stroke Program Early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised phase 3 trial (MR CLEAN). Lancet Neurol 2016;15:685-694.


Appendices
Appendix 1. Disclosure of conflicts of interest
Dr. Hidetoshi Matsukawa received a lecture fee from Daiichi-Sankyo and Stryker and consulting services fee from B. Braun.
Dr. Kazutaka Uchida received a lecture fee from Daiichi-Sankyo, Bristol-Myers Squibb, Stryker, and Medtronic.
Dr. Ilko L Maier: Speakers honoraria from Pfizer and Bristol- Myers Squibb.
Dr. Robert M Starke: RMS research is supported by the NREF, Joe Niekro Foundation, Brain Aneurysm Foundation, Bee Foundation, Department of Health Biomedical Research Grant (21K02AWD-007000) and by National Institute of Health (R01NS111119-01A1) and (UL1TR002736, KL2TR002737) through the Miami Clinical and Translational Science Institute, from the National Center for Advancing Translational Sciences and the National Institute on Minority Health and Health Disparities. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. RMS has an unrestricted research grant from Medtronic and Balt and has consulting and teaching agreements with Penumbra, Abbott, Medtronic, Balt, InNeuroCo, Cerenovus, Naglreiter, Tonbridge, Von Medical, and Optimize Vascular.
Dr. Marios-Nikos Psychogios: Grants from the Swiss National Science Foundation (SNF) for the DISTAL trial (33IC30_198783) and TECNO trial (32003B_204977), Grant from Bangerter-Rhyner Stiftung for the DISTAL trial. Unrestricted Grants for the DISTAL trial from Stryker Neurovascular Inc., Phenox GmbH, Penumbra Inc. and Rapid Medical Inc., Sponsor-PI SPINNERS trial (Funded by a Siemens Healthineers AG Grant), Research agreement with Siemens Healthineers AG, Local PI for the ASSIST, EXCELLENT, TENSION, COATING, SURF and ESCAPE-NEXT trials. Speaker fees: Stryker Neurovascular Inc., Medtronic Inc., Penumbra Inc., Acandis GmbH, Phenox GmbH, Siemens Healthineers AG.
Dr. Edgar Samaniego: Consultant for Medtronic, Microvention, Cerenovus and Rapid Medical.
Dr. Adam S. Arthur: Consultant for Arsenal, Balt, Johnson and Johnson, Medtronic, Microvention, Penumbra, Perfuze, Scientia, Siemens, Stryker.
Research support from Balt, Medtronic, Microvention, Penumbra and Siemens.
Shareholder Azimuth, Bendit, Cerebrotech, Endostream, Magneto, Mentice, Neurogami, Neuros, Perfuze, Revbio, Scientia, Serenity, Synchron, Tulavi, Vastrax, VizAI.
Dr. Shinichi Yoshimura received a lecture fee from Stryker, Medtronic, Johnson & Johnson, Kaneka Medics.
Dr. Hugo Cuellar: Dr. Hugo Cuellar: Consultant for Medtronic, Penumbra and Microvention.
Dr. Daniele G. Romano: Consultant for Penumbra, Balt, Microvention, Phenox.
Dr. Omar Tanweer: Consulting Agreements: Viz.AI, Inc., Penumbra, Inc, Balt, Inc, Stryker Inc, Imperative Inc. Proctor: Microvention Inc, Medtronic Inc.
Educational/Research Grants: Q’apel Inc, Steinberg Foundation
Dr. Adam Polifka: Consultant for Depuy Synthes and Stryker.
Dr. Charles Matouk: Consultant for Stryker, Medtronic, Microvention, Penumbra, and Silk Road Medical. Speaker for Penumbra and Silk Road Medical. Contact PI for NIH Grant R21NS128641.
Dr. Min S. Park: Consultant for Medtronic.
Dr. Michael R Levitt: Unrestricted educational grants from Medtronic and Stryker; consulting agreement with Medtronic, Aeaean Advisers and Metis Innovative; equity interest in Proprio, Cerebrotech, Apertur, Stereotaxis, Fluid Biomed, and Hyperion Surgical; editorial boards of Journal of NeuroInterventional Surgery and Frontiers in Surgery.
Dr. Richard Williamson: Consultant for Medtronic, Stryker, and Synaptive Medical.
Dr. Pedro Navia: Consultant for Penumbra, Medtronic, Stryker, Cerenovus and Balt.
Dr. Peter Kan: Grants from the NIH (1U18EB029353-01) and unrestricted educational grants from Medtronic and Siemens.
Consultant for Imperative Care and Stryker Neurovascular. Stock ownership in Vena Medical.
Dr. Reade De Leacy: Research grants from Siemens Healthineers and Kaneka medical. Consultant for Cerenovus, Stryker Neurovascular and Scientia Vascular. Minor equity interest Vastrax, Borvo medical, Synchron, Endostream, Von Vascular.
Dr. Shakeel A Chowdhry: Consultant and proctor for Medtronic and Microvention.
Dr. Alejandro Spiotta: Research support from Penumbra, Stryker, Medtronic, RapidAI, Avail. Consultant for Penumbra, Stryker, Terumo, and RapidAI. Equity Avail.
Dr. Sami Al Kasab: Grant from Stryker for RESCUE-ICAS registry.








