Epidemiology and Registry Studies of Stroke in Japan
Article information
Abstract
Stroke is the most prevalent cardiovascular disease in Japan. This review introduces two epidemiologic studies and four registry studies of stroke in Japan. The Hisayama Study was begun as a population-based prospective cohort study of cerebrovascular and cardiovascular diseases in 1961 in the town of Hisayama. Most of the deceased subjects of the study underwent autopsy examinations from the beginning of the study. Changes in stroke trends in the last 50 years were clarified by comparison of data from different study cohorts registered every 13 to 14 years. The Suita Study was based on a random sampling of Japanese urban residents. Several reports from this study showed the significance of pre-hypertension, as well as hypertension, as a risk factor for stroke by itself and in combination with other underlying characteristics. In addition, the Japan Multicenter Stroke Investigators' Collaboration (J-MUSIC), the Japan Standard Stroke Registry Study, the Fukuoka Stroke Registry, and the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement (SAMURAI) rt-PA Registry are explained as registry studies involving Japanese stroke patients.
Introduction
Stroke is the most prevalent cardiovascular disease and the most prevalent neurological disease in Asia.1 Many countries in East Asia and Southeast Asia have higher mortality rates from stroke than from ischemic heart disease, the opposite of Western countries.1 The prevalence of intracerebral hemorrhage (ICH) and intracranial arterial sclerosis is another unique feature of Asian patients.2,3 Among Asian countries, Japan was the first to become an aging society; the others, in particular Korea, have been rapidly approaching one. Thus, the epidemiologic characteristics of stroke in Japan seem to be good examples for other countries.
In this review, epidemiological studies and patients' registry studies of stroke in Japan are briefly introduced.
The Hisayama Study
The Hisayama Study was begun as a population-based prospective cohort study of cerebrovascular and cardiovascular diseases in 1961 in the town of Hisayama, a suburban community adjacent to the Fukuoka etropolitan area, Kyushu, in western Japan. Four study cohorts were established from Hisayama residents ≥40 years of age in 1961, 1974, 1988, and 2002 after screening examinations. One of the strengths of this study is that most of the deceased subjectsof the study underwent autopsy examinations from the beginning of the study (80% between 1962 and 1994),4 and thus, the morphological features of the brains examined by autopsy or brain imaging are available for most of the stroke cases in each cohort. The study was initiated to respond to the doubts of Western researchers in the pre-CT era that the very high mortality from ICH in Japan might be due to overdiagnosis of ICH. The autopsy results in the consecutive residents proved that the prevalence of ICH was not so high as was believed by Japanese physicians but also showed that ICH was still more common than ischemic stroke as a cause of death in Japan.5
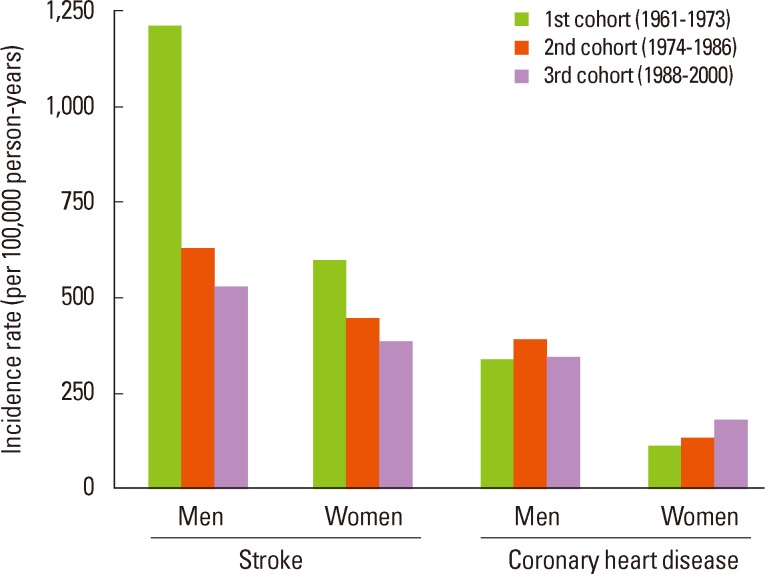
Of the many studies on stroke and other neurological diseases including dementia, those on stroke incidence and mortality are briefly introduced here. After 12-year follow-up for each of the first three study cohorts, the age-adjusted incidences of total stroke were 1,210 per 100,000 person-years for men and 598 for women in the first cohort (1961); they declined steeply in both sexes from the first to the second cohort (1974) and then declined relatively moderately in both sexes from the second to the third cohort (1988, Figure 1).6 Changes in the incidence among cohorts differed greatly between ischemic stroke and ICH. The incidence of ischemic stroke declined by 37% for men from the first to the second cohort, while the incidence of ICH declined by 61% for men. In contrast, the age-adjusted incidences of coronary heart disease were 340 per 100,000 person-years for men and 113 per 100,000 person-years for women in the first cohort, and they increased for both sexes in the newer cohorts, although they were much smaller than the stroke incidences in all of the cohorts. The different tendencies in the changes in incidence between stroke and coronary heart disease seem to be partly due to changes in prevalence of cardiovascular risk factors among the three cohorts: severe hypertension and current smoking became significantly less frequent, while glucose intolerance, dyslipidemia, and obesity became more frequent. Stroke mortality declined continuously as a result of changes in stroke incidence and significant improvements in acute stroke management; the age-adjusted stroke mortalities among the three cohorts were 634 (the first cohort: 1961), 232 (the second cohort: 1974), and 138 (the third cohort: 1988) per 100,000 person-years, respectively, for men and 286, 162, and 102 per 100,000 person-years, respectively, for women.
Among the ischemic stroke subtypes, the age-adjusted incidence of lacunar infarction declined significantly from the first to the third cohort for both sexes (5.68 per 100,000 person-years in the first cohort and 1.59 per 100,000 person-years in the third cohort for men during the 13-year follow-up), whereas the incidences of atherothrombotic and cardioembolic infarctions did not change during this period.7 As a result, the proportion of ischemic stroke subtypes differed greatly among the 3 cohorts; two-thirds of the male patients had lacunar infarction in the first cohort, compared to two-fifths in the third cohort. The high incidence in the first cohort and recent decline of lacunar infarction were similar to those for ICH, suggesting that intracranial small artery disease has been prevalent in the Japanese population and that the effect of recent developments in preventive therapy, especially antihypertensive therapy, are protective from development of the small artery disease.
Of the 410 patients in the first cohort who developed first ever stroke during 32-year follow-up, 108 (26%) experienced recurrent stroke within 10 years after the index stroke.8 The cumulative recurrence rates at 1, 5, and 10 years were: 10.0%, 34.1%, and 49.7% after ischemic stroke; 25.6%, 34.9%, and 55.6% after ICH; and 32.5%, 55.0%, and 70.0% after subarachnoid hemorrhage (SAH), respectively.
Of the 333 patients in the first cohort who developed first-ever stroke during 26-year follow-up, 268 (80.5%) died within 10 years after the index stroke, of whom 239 (89.2%) underwent autopsy examinations.9 The risk of death was greatest in the first year (men 40.3%; women 43.7%). The 30-day case fatality rate was substantially greater in patients with ICH (63.3%) or SAH (58.6%) than in patients with ischemic stroke (9.0%). The risk of dying after the index stroke was twelve times higher during the first year and two times higher during the overall 26-year period as compared to the risk for stroke-free controls. The most common cause of death was the index stroke in the first year, and the impact of recurrent stroke increased gradually thereafter.
The Hisayama Study is one ofthe first sophisticated epidemiological study and one of the most successful epidemiological study of cerebrovascular and cardiovascular diseases in the world. Several unique characteristics of Asian stroke patients were ascertained by this study. The Hisayama Study is still developing by expanding the target diseases into common nonvascular diseases and by adding genomic information for the analysis.
The Suita Study
Following the Hisayama Study, several epidemiological projects on cerebrovascular and cardiovascular diseases were started in Japan. Most of the study cohorts involved rural or suburban residents, since they are likely to continue to live in the area. The Suita Study was unique in that urban residents were registered.
Suita city, which contains the National Cerebral and Cardiovascular Center where the author works, is located adjacent to Osaka city, which is the second largest metropolitan area in Japan. The Suita Study was based on a random sampling of 12,200 Japanese urban residents. At baseline, participants between the ages of 30 and 79 years were randomly selected from the municipality's population registry and stratified into groups by sex and age in 10-year increments in 1989. Of these, 6,485 people underwent regular health checkups between 1989 and 1994. During an average 11.7-year (64,391 person-years) follow-up period, 213 strokes, consisting of 141 ischemic stroke, 32 ICH, 22 SAH, and 18unclassified strokes, and 133 myocardial infarctions were documented.10,11 Thus, the incidence of stroke did not differ much as compared to that of myocardial infarction in contrast to the high stroke incidence in the Hisayama Study (especially in its first cohort; the age-adjusted incidence of total stroke for menbeing 1,210 per 100,000 person-years and that of coronary heart disease being 340 per 100,000 person-years), although adjustments for age and other conditions are needed for accurate comparison between the studies. These findings suggest that the data from the Suita Study were influenced by the Western lifestyle, particularly diet.
Among the many publications from the Suita Study, those on the association between blood pressure (BP) levels and stroke incidence are briefly introduced here. The association between high-normal BP and cerebrovascular and cardiovascular disease had not been well studied in the Asian population. The percent ages of the participants with optimal, normal, and high-normal BP and hypertension Stage 1 and Stage ≥2, according to the ESH-ESC 2007 criteria, were 31%, 20%, 18%, 20%, and 11% for men and 42%, 17%, 16%, 16%, and 9% for women, respectively.9 Compared with the optimal BP group, the multivariate hazard ratios (HRs) (95% confidence intervals [CIs]) of stroke for normal and high-normal BP and hypertension Stage 1 and Stage ≥2 were 2.12 (1.04 to 4.30), 2.43 (1.21 to 4.86), 2.62 (1.35 to 5.09), and 4.38 (2.24 to 8.56) in men and 1.05 (0.49 to 2.24), 1.29 (0.63 to 2.67), 1.21 (0.61 to 2.45), and 2.20 (1.07 to 4.50) in women, respectively; the risk of myocardial infarction for each BP category was similar to that of stroke. Population-attributable fractions of high-normal BP and hypertension for combined stroke and myocardial infarction were 12.2% and 35.3% in men and 7.1% and 23.4% in women, respectively (Figure 2). These findings indicate the significance of pre-hypertension as a vascular risk factor and the necessity for pre-hypertensive patients to attempt to control BP through lifestyle modifications.

The HRs and positive fractions attributable to exposure to each blood pressure category at baseline for cardiovascular disease (including stroke): the Suita Study. The gray area displays the excessive incidence of CVD due to normal and high-normal blood pressures and hypertension stages 1 and ≥2 (From reference 10 with permission).
The combined impacts of BP categories and other risk factors were also thoroughly investigated in the Suita Study. A study on glucose abnormalities and that on chronic kidney disease (CKD) are summarized.11,12 The percentages of subjects with normoglycemia, impaired fasting glucose, and diabetes mellitus, defined according to the 2003 American Diabetes Association recommendations, were 59%, 35%, and 6% for men and 75%, 21%, and 4% for women, respectively.12 Compared with normoglycemic subjects, the multivariate HRs (95% CIs) for stroke were 1.11 (0.81-1.52) in individuals with impaired fasting glucose and 2.08 (1.29-3.35) in individuals with diabetes mellitus. Compared with normoglycemic and optimal BP subjects, increased risks of combined stroke and coronary heart disease were observed in the normoglycemic subjects with high-normal BP or hypertension, in impaired fasting glucose subjects with normal or higher BP, and in diabetic subjects regardless of BP category (P-value for interaction=0.046). The percentages of CKD subjects, defined as an estimated glomerular filtration rate (GFR) <60 mL/min/1.73 m2, using the Modification of Diet in Renal Disease equation modified by the Japanese coefficient (0.881), were 8.9% for men and 11.3% for women.10 Compared with the GFR ≥90 mL/min/1.73 m2 group, the HRs (95% CIs) for stroke were 1.9 (1.3 to 3.0) in the GFR 50 to 59 mL/min/1.73 m2 group and 2.2 (1.2 to 4.1) in the GFR <50 mL/min/1.73 m2 group. Compared with the optimal BP subjects without CKD, the normal BP, high-normal BP, and hypertensive subjects without CKD showed increased risks of stroke.However, the impact of each BP category on stroke (P for interaction: 0.03 in men, 0.90 in women) was more evident in men with CKD. These results show that pre-hypertension can be a stronger vascular risk factor when combined with other traditional and newer risk factors than when it is the sole risk factor.
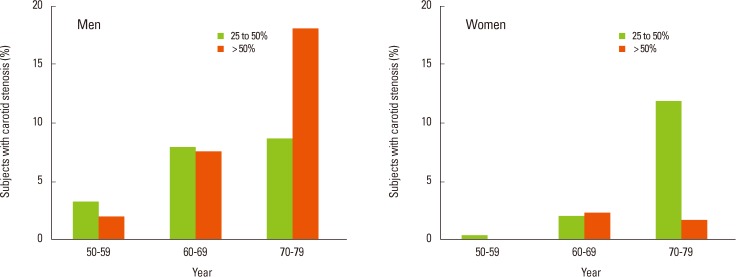
As is known, extracranial carotid atherosclerotic lesions are less frequent in the Asian population than in the Western population. The prevalence of asymptomatic extracranial carotid artery lesions and its relationship to cardiovascular risk factors were determined using ultrasound in the Suita residents.13 Significant sex differences were shown in the prevalence of atherosclerotic lesions in the extracranial carotid artery; 4.4% of all the subjects, 7.9% of the men, and 1.3% of the women aged 50 to 79 years had atherosclerosis accompanied by area stenosis >50%, and these values increased to 6.5%, 11.1%, and 2.1% for the subjects aged 60 to 79 years, respectively (Figure 3). In addition, accumulation of established major coronary risk factors (i.e., hypertension, smoking, and hypercholesterolemia) affected carotid atherogenesis in both sexes.14
Registry studies on stroke
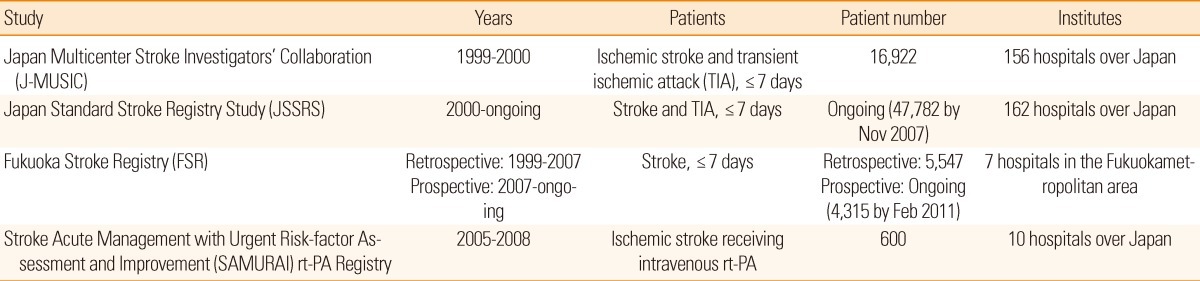
In this chapter, major registry studies on ischemic stroke in Japan are introduced (Table 1).
The Japan Multicenter Stroke Investigators' Collaboration (J-MUSIC) was a nationwide, multicenter, prospective, hospital-based registration study from May 1999 through April 2000, when intravenous recombinant tissue plasminogen activator (rt-PA) was not yet approved for clinical use. A total of 156 hospitals participated in the study, and 16,922 patients (70.6±11.5 years old) with acute ischemic stroke (94%) and transient ischemic attack (TIA, 6%) who were hospitalized within 7 days of onset were registered. As was common in the Asian population, lacunar stroke was the leading subtype (38.8%), followed by atherothrombotic (33.3%) and cardioembolic stroke (21.8%). The median National Institutes of Health stroke scale (NIHSS) score on admission was 5 (interquartile range 2 to 11), and 60.8% of the patients had a modified Rankin Scale (mRS)score of 0-2 at discharge, while 6.9% died during acute hospitalization.15 In the follow-up study of survivors, the 1-year cumulative mortality was 6.8%, which was relatively low compared to that from Western countries.16 The cause of death included cerebrovascular disease in 24.1%, pneumonia in 22.6%, heart disease in 18.1%, and cancer in 11.0%.
The Japan Standard Stroke Registry Study (JSSRS) is an ongoing multicenter stroke registration study based on a computerized database from 162 Japanese institutes. From January 2000 through November 2007, a total of 47,782 patients with acute stroke and TIA who were hospitalized within 7 days after onset was registered. Many subanalyses of the registry data have been reported in Japanese books published every two to four years. As the major findings, 75.4% of stroke patients had ischemic stroke, 17.8% had ICH, and the remaining 6.8% had SAH. As subtypes of ischemic stroke, 33.9% had atherothrombotic, 31.9% had lacunar, and 27.0% had cardioembolic stroke. It is interesting that the leading stroke subtype changed from lacunar stroke in J-MUSIC (1999-2000) to atherothrombotic stroke in JSSRS (2000-2007), although the participating hospitals and designs of the two studies were not identical. Effects of sex and age on stroke subtypes, underlying risk factors, initial conditions at onset, and outcomes of ischemic stroke patients were reported in English.17 Briefly, women were older than men at stroke onset (75.0±11.7 years versus 69.3±11.4 years), and women more frequently had cardioembolic events (odds ratio [OR] 1.090, 95% CI 1.036 to 1.146) after age-adjustment. Onset-to-arrival time was longer (β=0.0554, P=0.026), the initial NIHSS score was higher (β=0.1565, P<0.001), and duration of hospitalization was longer (β=0.0355, P=0.010) in women than in men after multivariate adjustment. At hospital discharge, women less commonly had an mRS score of 0-1 (OR 0.802, 95% CI 0.741 to 0.868) and more commonly had an mRS score of 4-6 (OR 1.410, 95% CI 1.293 to 1.537) than men. Thus, women developed more severe strokes than men in Japan.
The Fukuoka Stroke Registry (FSR) is an ongoing, multicenter, hospital-based registry in which acute stroke patients were enrolled from seven stroke centers in the Fukuoka metropolitan area. The FSR has the strengths that the database extensively collected underlying patients' information, image data principally using MRI/MRA, long-term follow-up of vital and functional conditions for years, and serological and genome genetic analyses for most participants. The associations of several risk factors, including pre-stroke glycemic control18 and admission proteinuria19 with clinical outcomes of ischemic stroke patients were published in the last couple of years. As a unique risk factor of ischemic stroke in Japanese, and probably in Korean people, a windblown sand dust originating from mineral soil in the deserts of China and Mongolia was significantly associated with the incidence of atherothrombotic brain infarction after adjusting for expected confounders, including meteorologic variables and other air pollutants in this cohort.20
Finally, let us consider the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement (SAMURAI) rt-PA Registry.21 This registry included 600 consecutive patients (377 men, 72±12 years old) with ischemic stroke and TIA who received intravenous rt-PA therapy in ten Japanese stroke centers that were balanced regionally between October 2005 (when intravenous alteplase therapy was approved in Japan) and July 2008. Symptomatic ICH within 36 hours with ≥1-point increase from the baseline NIHSS score developed in 3.8% of patients (95% CI 2.6 to 5.7%). At 3 months, 33.2% (95% CI 29.5 to 37.0%) of patients had an mRS score of 0-1, and the mortality was 7.2% (95% CI 5.4 to 9.5%). Analysis of 399 patients with a premorbid mRS score ≤1 who met the approved European indications(≤80 years old, an initial NIHSS score ≤24, etc.) showed that 40.6% (95% CI 35.9 to 45.5%) had a 3-month mRS score of 0-1. These percentages were similar to those in Western postmarketing surveys using 0.9 mg/kg alteplase. Several published subanalyses clarified the associations of risk factors and initial stroke features with thrombolysis outcomes.
The publications that were discussed in this review dealt with only a small part of each study, and the studies that were introduced represent only a small part of Japanese epidemiologic and registry studies. The author hopes that the readers of this journal will find the similarities (or differences) in stroke epidemiology between Japanese people and those in other countries of great interest.
Acknowledgements
I would like to thank Drs. Takanari Kitazono (Kyushu University), Yutaka Kiyohara (Kyushu University), Shotai Kobayashi (Shimane University), Yoshihiro Kokubo (National Cerebral and Cardiovascular Center), and Takenori Yamaguchi (National Cerebral and Cardiovascular Center) for the valuable advice.
Notes
The authors have no financial conflicts of interest.