Long-Term Functional Outcome for Patients Treated under Drip and Stay versus Drip and Ship Paradigm: A Single Network Experience
Article information
Dear Sir:
The implementation of telestroke networks significantly improved access to intravenous tissue plasminogen activator (IVtPA) in rural areas [1]. Through the telestroke system of care, patients who present to a community hospital (spoke) are evaluated using a videoconferencing platform by a stroke expert. Telestroke patients who receive IV-tPA either remain at the spoke (drip and stay) or are transferred to a tertiary medical center (drip and ship) [2].
We reviewed the prospectively collected data on all consecutive telestroke patients who received IV-tPA through the Medical University of South Carolina (MUSC) telestroke network between January 2016 and March 2018. Details on the MUSC telestroke network were described before [3]. Some spoke sites are able to keep stroke patients after receiving tPA (drip and stay), while other sites transfer all patients who receive tPA to a comprehensive stroke center (drip and ship). Drip and ship patients who were transferred to the hub for mechanical thrombectomy evaluation because of clinical suspicion for large vessel occlusion were excluded from this analysis. Our primary outcome was the modified Rankin Scale (mRS) at 90 days. A good functional outcome was defined as a 90-day mRS of 0–2.
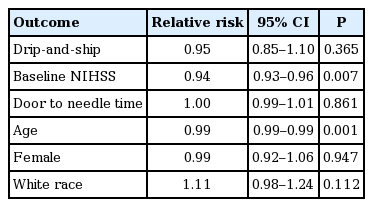
We assessed the predictors of having good 90-day outcome using a generalized linear model (GLM) with logit link controlling for age, sex, race, door to needle time and baseline National Institutes of Health Stroke Scale (NIHSS). Sensitivity analysis was done using worst-case scenario method to account for patients who were excluded from the GLM because of missing 90-day mRS (81 in the drip and stay group and 19 in the drip and ship group). This study was approved by the Institutional Review Board of the Medical University of South Carolina, with the need for written informed consent waived.
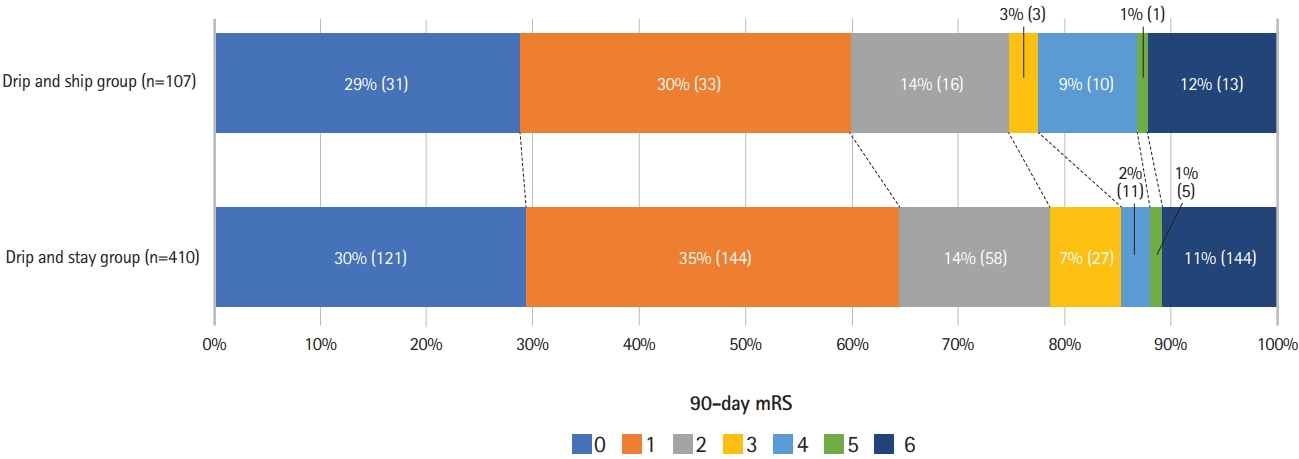
During the study period, 797 patients received tPA at spoke sites through MUSC telestroke network. Two hundred and eighty patients were excluded for missing data or because they were transferred to a thrombectomy-capable center for thrombectomy evaluation (Figure 1). A total of 517 patients were included in the analysis; 410 (79.3%) in the drip and stay group, and 107 (20.7%) in the drip and ship group. As shown in Table 1, there was no difference baseline NIHSS or door to needle time in both groups. A 90-day good functional outcome was achieved in 323 patients (78.8%) in the drip and stay and in 80 patients (74.8%) in the drip and ship group (P=0.372) (Figure 2). On multivariate analysis, we found no difference in the adjusted relative risk (RR) of having 90-day mRS ≤2 between drip and ship and drip and stay patients (RR, 0.95; 95% confidence interval [CI], 0.85 to 1.10; P=0.365) (Table 2). Similar results were found on sensitivity analysis using worst case scenario to account for patients with missing 90-day mRS (RR, 0.96; 95% CI, 0.83 to 1.11; P=0.572).
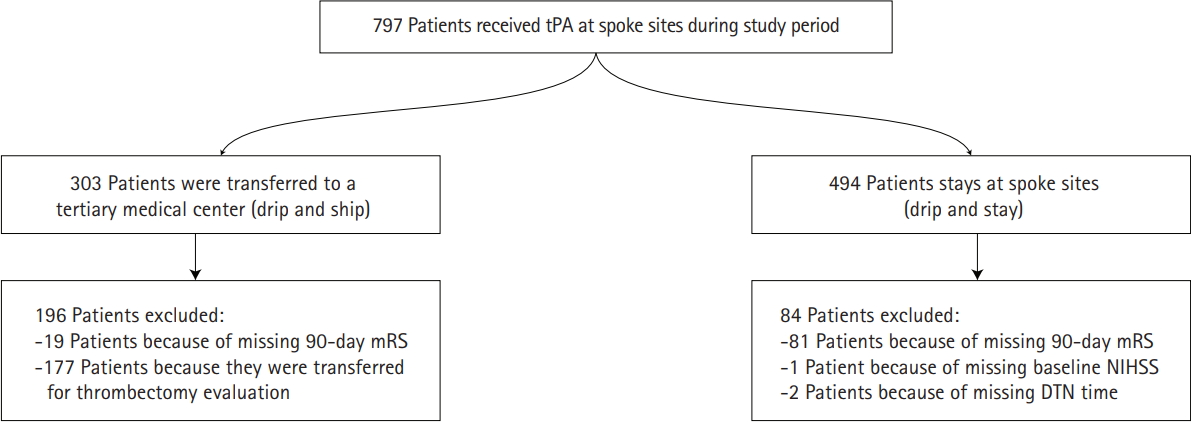
Study flowchart. tPA, tissue plasminogen activator; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; DTN, door to needle.
Our study shows that patients treated with intravenous alteplase through telestroke and who otherwise do not require a higher level of care can remain at spoke centers and can have excellent outcomes that are comparable to those transferred to a tertiary medical center.
Early experience with tPA demonstrated that mortality was higher when tPA was administered in inexperienced hospitals, which led to more support for telestroke networks to be able to provide a safe and efficient solution for acute stroke management [4,5]. With more evidence emerging concerning the benefits of telestroke consultations, including higher rates of thrombolysis [6], one of the main questions remaining is whether stroke patients post-tPA will experience better outcomes if they stay at the spoke sites (drip and stay) or if they are transferred to a tertiary medical center (drip and ship). This question is especially important for patients who are not candidates for endovascular or neurosurgical intervention. A few studies in the past have tried to answer this question, including a study by Yaghi et al. [7] which demonstrated that telestroke patients with mild stroke (NIHSS <8) have similar long-term outcomes whether they stay at a spoke or are transferred to a primary stroke center. However, patients with moderate to severe stroke (NIHSS ≥8) had higher odds of having a good long-term outcome if they are transferred to the telestroke hub [7]. Our study has shown similar results with an advantage that the comparison groups were more homogeneous in terms of stroke severity given that all patients with suspected or confirmed large vessel occlusion were excluded from the study.
After the extension of the mechanical thrombectomy treatment window, more patients are expected to be transferred to thrombectomy-capable centers for thrombectomy evaluation and treatment [8]. Thus, new strategies should be put in place to ensure that only patients who will benefit from the transfer are being transferred. With the cumulative evidence that has shown that telestroke patients may have good outcomes when they remain at spoke sites following thrombolysis [5,9], more efforts should be taken to ensure that patients who are treated under the drip and stay paradigm receive equivalent care as patients who are treated under the drip and ship paradigm.
Our study has a few limitations. First, although the telestroke log at MUSC is prospectively maintained, the study parameters were reviewed retrospectively. Second, 90-day mRS was missing for 100 patients. However, sensitivity analysis using worst case scenario showed similar results to the primary multivariate analysis. Finally, we were unable to control for factors that affected the decision for transfer to a tertiary medical center including spoke hospital staffing, presentation during off-hours and other medical complications.