Stroke in the Time of Coronavirus Disease 2019: Experience of Two University Stroke Centers in Egypt
Article information
Dear Sir:
In the beginning of year 2020, the world was hit by a pandemic of coronavirus disease 2019 (COVID-19), thus posing a significant challenge to health care systems worldwide [1]. Consequently, emergency doctors tend to avoid hospital admission of patients with risk factors because of the higher mortality rate if this population is exposed to COVID-19 infection [2]. Nevertheless, non-communicable diseases, as acute stroke, are still there in the background of this pandemic and definitely need to be efficiently managed. This implies that acute stroke management pathways ought to be revised to maintain proper stroke care while protecting patients and health care providers from contracting COVID-19 [3].
In this study we discuss the modified pathway implemented in the two stroke centers of Ain Shams University (ASU) hospitals. We also evaluate its efficacy by comparing patient outcome over 50 days, since the declaration of the first COVID-19 case in Egypt on 15th of February, with a similar immediately antedating time duration.
In this context modifications were implemented in ASU by assigning one of its three hospitals as a COVID-hospital. In the other two non-COVID hospitals, the emergency room was moved to a frontline building away from the inpatient sectors. This is where patient triage takes place with personal protective equipment provided to medical and para-medical personnel, including full sleeved gown, surgical mask, face shield and extended cuff gloves beside a N95 respirator for aerosol-generating procedures. A computed tomography (CT) machine was dedicated for suspected cases, with sterilization between sessions. Also a thrombectomy suite and an isolation unit were assigned for suspected cases. After receiving appropriate management, cases proven positive by swab are immediately transferred to the COVID hospital (Figure 1).

Modified acute stroke pathway of Ain Shams University stroke centers during the coronavirus disease 2019 (COVID-19) pandemic. ER, emergency room; CT, computed tomography; CTA, computed tomography angiography; rtPA, recombinant tissue plasminogen activator.
Statistical analysis was done using SPSS version 16 (SPSS Inc., Chicago, IL, USA). Detailed methods are available in Supplementary methods.
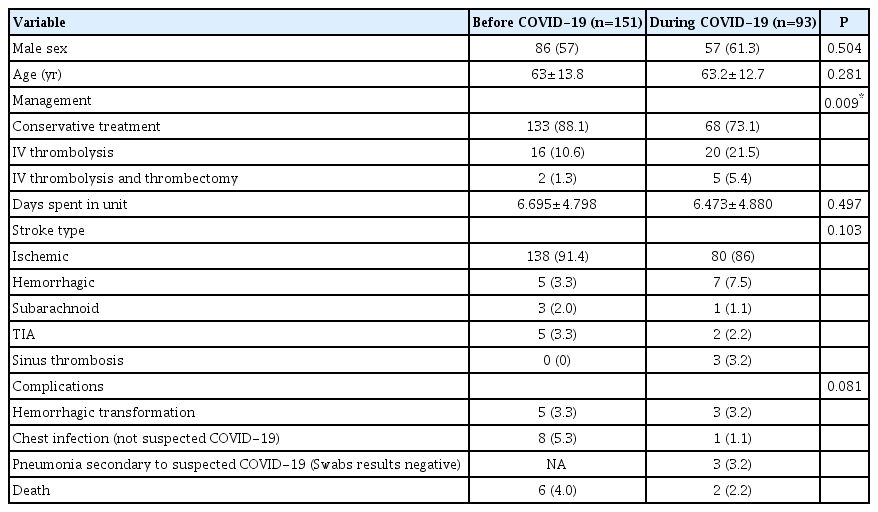
Outcome in COVID-19 compared to pre-COVID-19 period: despite that the total number of cases admitted in COVID period (n=93) was less than pre-COVID (n=151), however percentage of thrombolytic therapy was significantly higher (21.5% and 10.6% respectively, P=0.009), so was the percentage of thrombectomy (5.4% and 1.3% respectively). As for stroke subtypes, hemorrhagic strokes and sinus thrombosis were more in the COVID period (7.5%, 3.2%, respectively), while in pre-COVID (3.3%, 0%, respectively).
Complications were notably yet non-significantly less in the COVID period (9.7%) as compared to pre-COVID (12.6%). Total percentage of chest infection was slightly higher in preCOVID (5.3%) compared to (4.3%) in COVID period. All three cases suspected to have COVID pneumonia proved negative by swab, so no patients were transferred to COVID hospital. Also death rate was more in pre-COVID (4%) versus in COVID period (2.2%) (Table 1).
The COVID-19 period onset-to-door time was significantly less (median 240 minutes compared to 600 minutes pre-COVID period; P<0.001). However, door-to-needle time was almost equal in both time periods (Table 2).
National Institutes of Health Stroke Scale (NIHSS) baseline was significantly higher in COVID period compared to preCOVID (median 7 and 5 respectively, P=0.02). NIHSS and modified Rankin Scale (mRS) were nearly similar at discharge (Table 2). Out of 50 cases arriving beyond therapeutic window in COVID period; the commonest cause of delay was wake up stroke 30.9%, while fear of catching COVID-19 or of unavailability of stroke service was 10.9%.
Three years ago, since the implementation of the acute stroke protocol in our stroke centers, the rate of revascularization therapy has increased up to about 5 folds [4]. Thus, since the emergence of COVID-19 in Egypt, our main concern was to keep the acute stroke service running with the same efficiency. The results of the current study showed that some stroke patients refrained from seeking emergency treatment at hospitals for fear of infection, which explains less number of admitted stroke patients and higher NIHSS denoting severe stroke. It is possible that patients with minor stroke in the COVID period tend to decline from seeking help at hospitals. This goes with the conclusion of the European Stroke Organization in a survey among 55 countries that fear from becoming infected kept patients from seeking help [5]. In spite of that the rate of thrombolytic and bridging therapy was higher possibly due to shorter transportation time and availability of caregivers due to curfew and lock down and consequently shorter onset-to-door time. While the relatively longer door-to-needle time, reaching a maximum of 60 minutes, as compared to a maximum of 40 minutes pre-COVID is attributable to more steps taken on admission including CT chest and nasopharyngeal swab.
Type of stroke did not show significant difference, yet there is a trend towards more hemorrhagic strokes and sinus thrombosis. Whether this is due to disturbance of coagulation profile attributable to undetected COVID-19, needs to be verified.
Finally, complications seem to be less during the COVID period which can be due to heightened infection control measures taken in the whole hospital. To our knowledge this is one of the first studies to set a comparative analysis of acute stroke service pre- and during the declaration of the COVID-19 pandemic.
In conclusion, acute stroke management is a dynamic process that is subject to modification according to changing and challenging situations. Implementation of a modified stroke pathway compatible with infection control measures in our stroke centers resulted in an overall outcome similar in efficiency to the pre-COVID pathway.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2020.01550.
Notes
This study was carried out in the both stroke units of Ain Shams University hospital and Ain Shams University specialized hospital in Abbasia Square, Cairo, Egypt.
Disclosure
The authors have no financial conflicts of interest.