Simple but Organized Neurology Residency Training Improves the Quality of Acute Stroke Care: From the Outset to Long-Term Effect
Article information
Dear Sir:
Acute stroke team often requires a competent and confident neurologist who plays a decisive role in managing acute stroke patients. At teaching hospitals in Taiwan, the training program for acute stroke care runs throughout the entire residency, which means that junior residents have the opportunity to manage acute stroke patients in the emergency department (ED) under the supervision of experienced stroke physicians and fellows. Residents usually need to handle the details of treatment, such as providing the explanation, obtaining treatment consent, and prescribing drugs. Previous report showed that neurology residency program increased the thrombolysis utilization in acute stroke [1], but the lack of experience of resident doctor may potentially cause a delay in the acute stroke treatment. Junior residents accumulate experience from case management throughout their residency [2]. The learning curve is therefore random, time-dependent and motivation-dependent. Here, we report a simple but integrated training program for junior neurology residents and the outcome in terms of improvement in acute stroke treatment in a tertiary medical center in Taiwan. The study was approved by the Institutional Ethics Review Board of NCKUH (B-ER-102-097).
National Cheng Kung University Hospital is a 1,320-bed tertiary medical center and a comprehensive stroke center capable of providing intravenous thrombolysis (IVT) and endovascular thrombectomy (EVT). It is a teaching hospital that provides residency training, and it provides training to 10 to 12 junior to senior neurology residents, approximately 1 to 3 first-year residents every year. For acute stroke management, code stroke activation at the ED was started in 2008, and we reorganized a work flow for IVT treatment to enhance the acute stroke care quality in 2015.
Before July 2018, our residents received the traditional training course by the regulation of Taiwan Neurological Society. Since August 2018, we initiated a series of training programs (Supplementary data), including routine monthly guideline club, online video-assisted National Institutes of Health Stroke Scale (NIHSS) training courses, and a test simulating an acute stroke scenario. Residents were also required to obtain NIHSS certifications, the Advanced Neurological Life Support (ANLS) license and a certification on preparing the tissue plasminogen activator (tPA) solution by themselves from powder in their first year of residency. Finally, the junior residents were permitted to attend the ED work shift after passing the simulating test and acquiring all the certifications.
Between August 2015 and October 2020, we divided the residents into two groups: the control group (C group) comprised residents who had not received the new educational program prior to attending the ED work shift, whereas the intervention group (I group) comprised residents who had completed the requirement. To evaluate the efficacy of the training programs on the quality of acute stroke care, the average door-to-needle (DTN) time and the percentage of patients with a DTN time ≤60 minutes were compared between residents in the C and I groups in their junior residency (defined as the second year of residency) and in their senior years (defined as the third or fourth year of residency).
Data of 115 patients who were managed by 17 residents (C:I group = 9:8) were analyzed. Regarding tPA administration in junior residency year, the I group displayed a lower mean DTN time (I:C group = 53:65 minutes, P<0.05) and a higher percentage of patients with a DTN ≤60 minutes than the C group (I:C group = 78%:53%, P<0.05) (Table 1). Figure 1A and Supplementary Table 1 showed the trend of average DTN time significantly improved after introducing the training programs.
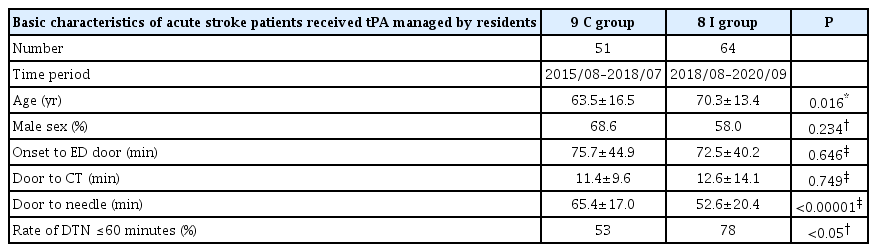
Comparison of baseline characteristics of acute stroke patients managed by residents of control and intervention group
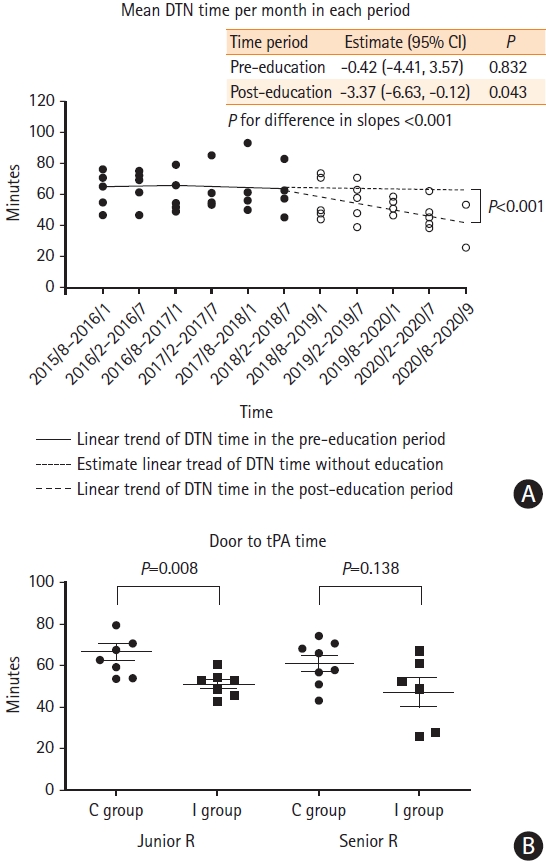
(A) Trend over time for the average door-to-needle (DTN) time per month in serial periods before and after introducing the training programs (before and after August 2018). (B) Comparison of average DTN time between I and C groups in their junior and senior residency. DTN time was significantly lower in the I group than in the C group during both junior residents and senior residents. Statistical analysis was performed using the Mann-Whitney U test. Statistical significance was defined at P<0.05. CI, confidence interval; tPA, tissue plasminogen activator.
The change in performance from junior to senior residency is presented in Figure 1B. Each spot represents as the average DTN time for each resident. The I group significantly outperformed the C group during the junior residency (P=0.008). The residents in the C group improved their performance in the senior residency. However, the residents in the C group had also spent a longer time in the senior residency than those in the I group, although the difference was not statistically significant.
From this study, a simple but integrated programs significantly improved the performance of residents with regard to managing acute stroke in their junior residency, and the program had a long-term positive effect. Improvement in the clinical performance of the residents also improved the quality of acute stroke care.
Monthly guideline or journal readings provides basic knowledge of standard stroke treatment. The license requirement of NIHSS, ANLS and tPA preparation ensures the clinical competence. Through simulations, residents could experience clinical scenarios and formulate treatment plans. Experiencing these simulations and preparing plans to solve clinical problems helped the learners overcome similar situations when they encountered them in the future. Analysis of the post intervention results indicates that our education program reached the Kirkpatrick level 4. It successfully reduced the time spent in treating acute stroke with IVT under the same tPA protocol in the ED.
Studies on stroke management have emphasized the benefits of protocol revision [3]. We revised the acute stroke protocol regarding IVT in 2015, and the new protocol revision only incorporated EVT starting in 2018. Therefore, the improvement of the performance of our residents did not contribute to the revision of the acute stroke protocol. We found that the reduction in the DTN time was not attributable to reductions in the onset-to-door time or door-to-computed tomography time, which indicates that the DTN reduction did not solely originate from the public awareness of acute stroke treatment or adequate organization of the in-hospital process due to a mature tPA protocol in the ED. The DTN time reduction may be due to the more rapid clinical decision making and treatment initiation among the I group compared with the C group. The clinical performance shown in Figure 1A confirms that the effect of our education program on acute stroke management by neurology residents was positive from the outset, and the learners showed retention and steady growth, continuing to improve in senior residency.
In conclusion, our report suggests that organized educational intervention regarding acute stroke enhance the clinical performance of neurology residents since junior residency, and thereby the quality of acute stroke care.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2020.04910.
Mean DTN time per period after adjusting calendar year by linear regression analysis
Acknowledgements
We thank Stroke Center, and Department of Neurology in National Cheng Kung University Hospital (NCKUH) for planning and executing the education program. We thank NCKUH for funding this work. We are grateful to the Biostatistics Consulting Center, NCKUH for providing us with statistical consulting services. The study was funded by NCKUH (NCKUH-10902039).
Notes
The authors have no financial conflicts of interest.
