Early Administration of Edoxaban After Acute Ischemic Stroke in Patients With Non-valvular Atrial Fibrillation: A Pilot Randomized Trial
Article information
Dear Sir:
Without anticoagulation, the risk of early recurrence in the first 14 days after atrial fibrillation (AF)-related ischemic stroke is approximately 0.5%–1.3% per day [1]. Anticoagulation is an essential strategy for preventing recurrent stroke in patients with AF-related stroke. However, it increases the incidence of intracranial hemorrhage (ICH) in the early stages of stroke. For the timing of anticoagulation, the “1–3–6–12 days rule” has been used: administration of anticoagulant at day 1 for transient ischemic attack (TIA), day 3 for mild stroke (National Institutes of Health Stroke Scale [NIHSS] <8), day 6 for moderate stroke (NIHSS 8–16), and day 12 for severe stroke (NIHSS >16) [2]. However, this rule was established when vitamin K-dependent anticoagulation was used. Non-vitamin K-dependent oral anticoagulants (NOACs) have a similar efficacy and are associated with a lower bleeding risk [3]; they may be administered earlier than warfarin in patients with acute ischemic stroke (AIS) [4]. However, no randomized controlled trials have focused on the timing of NOAC administration in patients with AF-related AIS. The purpose of this study was to examine the feasibility and possible efficacy of NOAC administration at timepoints earlier than the conventional rules. Considering that early recurrent infarcts identified using diffusion-weighted imaging (DWI) and ICH identified using gradient-echo imaging (GRE) are common in patients with AF-related AIS [5], we used these imaging endpoints in this pilot study.
This was a multicenter, randomized, open-label, blinded endpoint trial. Patients with AIS identified by DWI were included if they (1) were ≥20 years old, (2) had cardioembolic infarction (due to AF) identified before randomization, (3) had mild to moderately severe stroke (TIA and severe strokes were excluded), and (4) could be administered edoxaban within 48 hours of symptom onset. The exclusion criteria are summarized in Supplementary Table 1. Patients were randomized to either the conventional edoxaban treatment group (C-group) or the early edoxaban treatment group (E-group). In the C-group, a standard dose of edoxaban was administered to patients on day 3 for mild stroke and on day 6 for moderate stroke after symptom onset. Before administration of edoxaban, the use of anticoagulants was prohibited. In the E-group, a half-dose of edoxaban was administered from onset until day 3 (for mild stroke) or day 6 (for moderate stroke), and a standard dose of edoxaban was then administered as in the C-group. Baseline magnetic resonance imaging (MRI) was performed 24–48 hours after symptom onset, and follow-up MRI was performed between days 10 and 14. MRI images, including DWI, GRE, fluid-attenuated inversion recovery, and magnetic resonance angiography, were collected at the Asan Medical Center Central Image Laboratory and read by neuroradiologists blinded to treatment allocation. Thrombolysis or endovascular therapy was permitted if appropriate. Edoxaban was administered 24 hours later to patients who received thrombolysis therapy. This trial was performed in accordance with the Good Clinical Practice guidelines and approved by the Institutional Review Boards of all participating centers. Written informed consent was obtained from all patients (clinicaltrials.gov–NCT03433235).
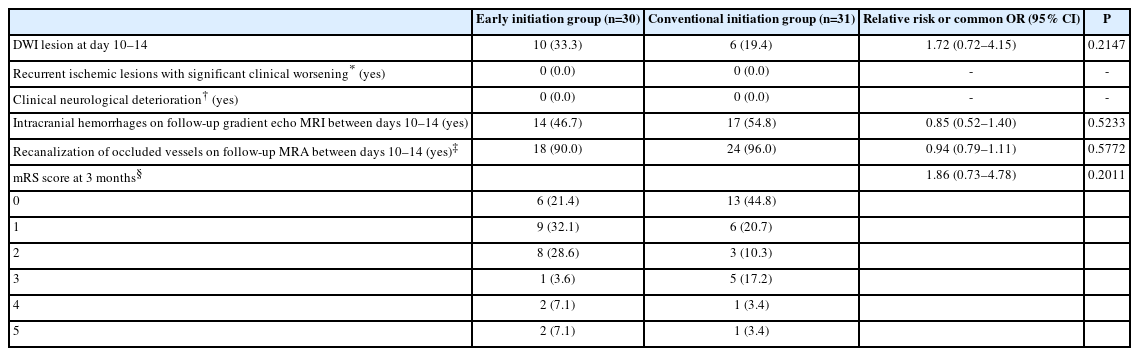
The primary outcome was the occurrence of new symptomatic or asymptomatic infarcts detected on DWI on days 10–14, in comparison with the baseline DWI findings at 24–48 hours. Secondary endpoints included (1) recurrent infarcts that were associated with clinical deterioration (increased NIHSS ≥4) within 10–14 days, (2) neurological deterioration (increased NIHSS ≥2), (3) any ICH detected by GRE at days 10–14, (4) recanalization of the occluded vessels in patients who did not undergo thrombolysis or endovascular therapy, and (5) functional status (modified Rankin Scale [mRS]) at 3 months. Although the sample size could not be calculated for this exploratory trial, a total of 66 patients were enrolled.
The primary and secondary endpoints were assessed in the modified intention to treat (ITT) population, which included patients who were randomized and completed follow-up MRI. Per-protocol analysis was performed in patients who had no major protocol violation and took ≥80% of the assigned study medications. Adverse events were assessed in the safety population, i.e., those who received at least 1 dose of study drugs. For statistical analysis, chi-square test, Fisher’s exact test, or CochranMantel-Haenszel shift test was performed using SAS 9.4 software (SAS Institute, Cary, NC, USA).
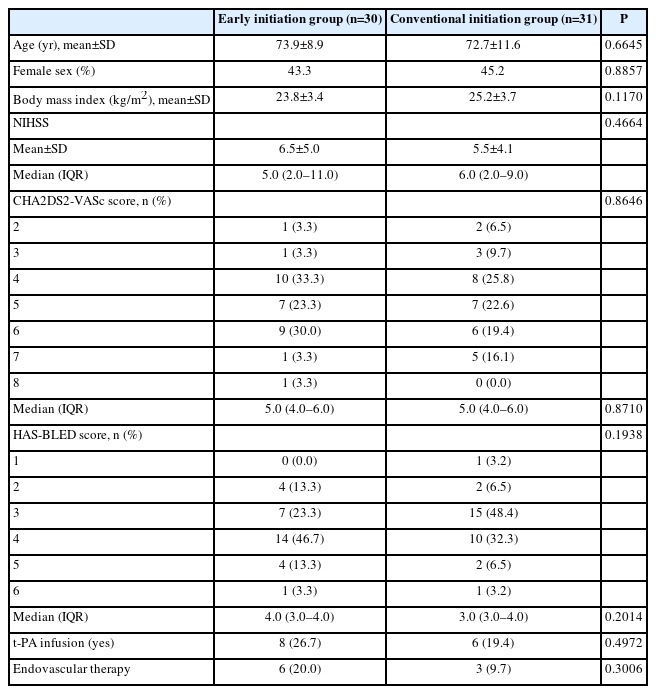
In total, 66 patients (E-group, n=33; C-group, n=33) were enrolled from four hospitals (Asan Medical Center, Kyung Hee University Hospital, Soonchunhyang University Hospital, and Dong-A University Hospital). Thirty patients from the E-group and 31 from the C-group were included in the ITT group. There were no differences between the E-group and C-group in terms of demographic characteristics, baseline NIHSS, CHA2DS2-VASc score, HAS-BLED score, and the incidence of thrombolysis/endovascular therapy (Table 1). With respect to the primary endpoint (Table 2), DWI-identified ischemic lesions occurred at 10–14 days in 10 (33.3%) and 6 (19.4%) patients in the E-group and C-group, respectively (relative risk 1.72, 95% confidence interval: 0.72–4.15, P=0.2147). All lesions were asymptomatic and none were associated with clinical deterioration. The results obtained using the per-protocol analysis were similar. ICH detected by GRE occurred in 14 (46.7%) and 17 (54.8%) patients in E-group and C-group, respectively, and all were asymptomatic microbleeds (<1 cm in diameter). The neurological deterioration rate, recanalization rate, and mRS score did not differ between the groups (Table 2).
We found that the administration of a half-dose of edoxaban earlier than the conventional strategy was safe and feasible, at least in patients with mild to moderately severe AIS. Contrary to our expectations, DWI-identified ischemic lesions occurred in 10 (33.3%) and 6 (19.4%) patients in the E-Group and C-Group, respectively. The prevalence of new MRI-identified lesions was generally in line with the findings of a previous study [5]; 29.5% and 35.6% of the patients in the rivaroxaban and warfarin groups, respectively, had such lesions at 4 weeks. Because we focused on feasibility and safety in this pilot study, we administered a halfdose, rather than full dose, of edoxaban to the E-group patients during the early period, which was associated with lower bleeding risk than the full dose [6]. The half-dose of edoxaban we used might have been insufficient in preventing recurrent MRI-identified ischemic lesions in these high-risk patients. Although the small sample size in this study did not allow us to interpret the results, the trend of an increased incidence of DWI-identified lesions in the E-group needs to be investigated in future research. During the process of this manuscript, a randomized trial was published that showed that early (≤4 days) NOAC initiation was non-inferior to delayed (5–10 days) initiation in patients with AIS. However, there were no differences in the mortality and recurrent stroke rates between the two groups [7]. Currently, three other randomized clinical trials, ELAN (Early versus Late initiation of direct oral Anticoagulants in post-ischaemic stroke patients with atrial fibrillatioN) [8], OPTIMAS (OPtimal TIMing of Anticoagulation After Acute Ischaemic Stroke) [9], and START (Optimal Delay Time to Initiate Anticoagulation After Ischemic Stroke in Atrial Fibrillation) [10] are undergoing to determine the optimum start time of anticoagulation in AF-associated AIS, which will hopefully provide more definitive answer.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2023.00325.
Exclusion criteria
Notes
Funding statement
This study was funded by Daiichi Sankyo Korea Co., Ltd. The funder had no role in the design or conduct of the study.
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: JSK. Study design: JSK. Methodology: JSK. Data collection: JSK, KBL, DIC, JKC. Investigation: JSK, KBL, DIC, JKC. Statistical analysis: JSL. Writing—original draft: JSK. Writing—review & editing: JSK, KBL, DIC, JKC. Funding acquisition: JSK. Approval of final manuscript: all authors.
Acknowledgements
This study was performed and reported according to Good Clinical Practice guidelines and the Declaration of Helsinki, and the protocol was reviewed and approved by the review boards of Asan Medical Center, Soochunhyang University Hospital, Kyung Hee University Hospital, and Dong-A University Hospital, with approval numbers 2018-0033, 2017-12-003, 2018-01-008, and DAUHIRB-19-140, respectively. Written informed consent was obtained from all eligible patients or their legally authorized representatives.