Antithrombotic Management of Patients with Nonvalvular Atrial Fibrillation and Ischemic Stroke or Transient Ischemic Attack: Executive Summary of the Korean Clinical Practice Guidelines for Stroke
Article information
Abstract
Cardioembolic stroke related to nonvalvular atrial fibrillation is associated with a high recurrence rate and high mortality and morbidity. In this population, therefore, optimal anticoagulant therapy is required to prevent the occurrence of second stroke. Oral anticoagulant, warfarin has been traditionally used, but it is greatly limited by its narrow efficacy window, complex pharmacokinetics, and multiple drug interactions, thus requiring frequent blood monitoring. Recently, oral anticoagulants targeted for a specific coagulation component have been newly developed and tested in large clinical trials. Dabigatran, direct thrombin inhibitor, and rivaroxaban, apixaban, and edoxaban, inhibitors of factor Xa harbor great merits of rapid action time, short half-life, stable plasma concentration, and little drug interaction. Recently, large randomized clinical trials and meta-analyses have been published to show the efficacy and safety of the new oral anticoagulants compared with warfarin. Based on the results from recent clinical trials, we revised recommendations to apply optimal anticoagulant therapy in patients with nonvalvular atrial fibrillation and ischemic stroke or transient ischemic attack.
Introduction
Large nationwide multicenter stroke registry studies in Korea have shown an increase in cardioembolic stroke, which accounts for 20% of all ischemic strokes,1 and found that 19% of patients with ischemic stroke have atrial fibrillation.2 Cardioembolic stroke is also highly associated with severe neurological deficits, early and late embolic recurrences, and a high mortality. The most common cause of cardioembolic stroke is atrial fibrillation, the prevalence of which robustly increases with age.3 Risk factors including congestive heart failure, old age, hypertension, diabetes mellitus, and previous stroke further increase the risk of stroke, and these risk factors are prevalent in patients with stroke. Therefore, anticoagulation is highly recommended for secondary stroke prevention in patients with nonvalvular atrial fibrillation without contraindications. Warfarin has traditionally been used for long-term therapy. A conventional oral anticoagulant, warfarin confers its anticoagulant effect by inhibiting vitamin K-dependent factors (II, VII, IX, X). However, warfarin use is challenging for physicians and patients on account of its narrow therapeutic window, the need for frequent blood testing, its unstable anticoagulation effect, inter- and intra-individual variability of action, and multiple drug and food interactions. Several oral anticoagulants targeting a specific coagulation factor have been developed recently. Dabigatran etexilate is rapidly converted into active dabigatran by plasma carboxyesterases and competitively and reversibly inhibits both thrombin activity and generation. Rivaroxaban, apixaban, and edoxaban are not prodrugs, and competitively and reversibly bind to the active site of factor Xa. The new anticoagulants have the advantages of rapid action, a short half-life, stable plasma concentration, and little drug interaction, and have been tested in large randomized clinical trials. The first edition of the secondary stroke prevention guidelines for patients with atrial fibrillation was published in 2009, reflecting evidence published through June 30, 2007. However, large randomized clinical trials, subgroup analyses, and meta-analyses of the efficacy and safety of the new oral anticoagulants (NOACs) have been published recently. Accordingly, the guidelines writing committee revised the recommendations for preventing secondary stroke in patients with atrial fibrillation.
Previous guideline
The first edition of the secondary stroke prevention guidelines for patients with atrial fibrillation was published in 2009 and did not reflect evidence concerning the newly developed oral anticoagulants. The previous recommendations were as follows:
Warfarin treatment (INR 2.0-3.0) is recommended, unless contraindicated, in patients with ischemic stroke or transient ischemic attack coexisting with sustained or paroxysmal atrial fibrillation (Evidence level: Ia, Recommendation grade: A).
If anticoagulants cannot be used, aspirin can be used instead (Evidence level: Ia, Recommendation grade: A). The recommended daily dose of aspirin is 325 mg. In Korea, a prescribable dose of 300 mg may be considered (Evidence level: IV, Recommendation grade: GPP).
For the recurrence of ischemic stroke or transient ischemic attack in atrial fibrillation patients already receiving adequate anticoagulation therapy, increasing the therapeutic target to INR 2.5-3.5 or initiating combination therapy with antiplatelets may be considered (Evidence level: IV, Recommendation grade: C).
Methodology
Organization of the Korean Clinical Practice Guidelines Committee
Recommendations of the Korean Clinical Practice Guidelines (CPG) for Stroke are generated by summarizing foreign and Korean published evidence modified to take the Korean health care system into account. The first edition was published in 2009 and reflects evidence published through June 30, 2007. Since then, the Steering Committee has monitored new clinical evidence and selected topics requiring guidelines updates. The Steering Committee makes a final decision regarding guideline updates and appoints a Writing Committee chair for each of the following three areas: primary stroke prevention, acute stroke management, and secondary stroke prevention. Each chair organizes writing members by referring to their specialty with the approval of the Steering Committee. Under the supervision of each chair, the Writing Committee members search, compile, and evaluate new evidence and make recommendations for each topic. With the advent of new evidence for antithrombotic management in atrial fibrillation, the Steering Committee decided to update the guideline for secondary stroke prevention in patients with atrial fibrillation and composed the Writing Committee. Disagreements among Writing Committee members were resolved by consensus. The Steering Committee reviewed the first draft and recommended revision if necessary. The Writing Committee's revised draft was submitted, reviewed, and finally approved by the Steering Committee.
Evidence search process
The update process adheres to the international tool for the assessment of practice guidelines, the Appraisal of Guidelines for Research & Evaluation (AGREE II). The process of guideline development requires the documentation of all literature searches performed for the guideline revision. The search form to be completed by the Writing Committee includes items such as search duration, publication type, key words, search strategy, and database. For this revision, we searched articles from MEDLINE/PubMed and the National Guideline Clearinghouse from July 2007 to May 2014 using the following key words: atrial fibrillation AND stroke OR transient attack AND anticoagulant AND dabigatran OR rivaroxaban OR apixaban OR edoxaban AND warfarin AND stroke. Key words for exclusion included catheter ablation, cardioversion, valve replacement surgery, and left atrial appendage closure. The studies were limited to randomized controlled trials, controlled clinical trials, meta-analyses, and guidelines.
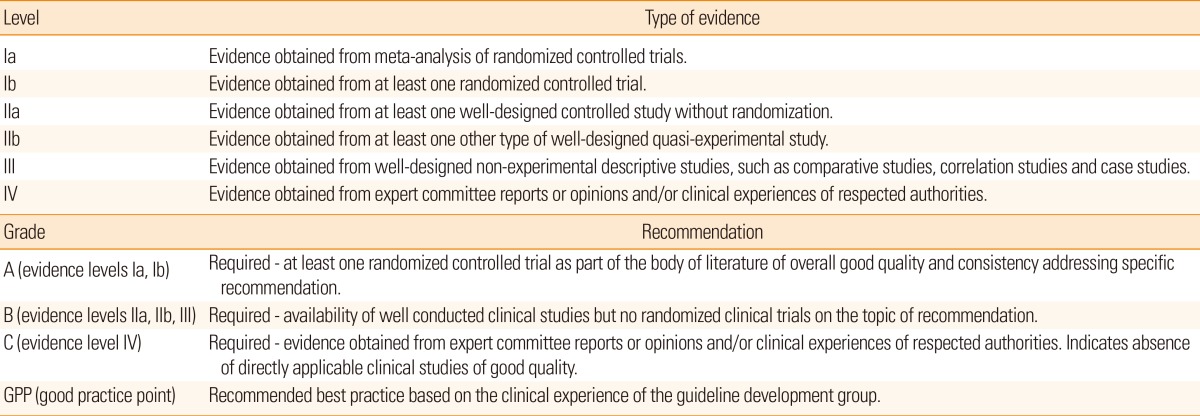
Evidence review and determination of recommendation level
The Writing Committee reviewed all available studies meeting the inclusion and exclusion criteria, and finally retrieved 8 randomized controlled trials, 5 meta-analyses, and 4 subgroup analyses. The Writing Committee additionally reviewed 3 foreign updated guidelines including those of the European Society of Cardiology (2012),4 the American College of Cardiology/American Heart Association (2014),5 and the American Stroke Association (2014).6 Then, the level of evidence and the grade of each recommendation were determined according to the format suggested by the US Agency for Healthcare Policy and Research (currently the Agency for Healthcare Research and Quality, AHRG) in 1993 (Table 1). The level of evidence indicates the quality and strength of the cumulative scientific evidence, and the grade of recommendation implies how strongly a statement is recommended.
Revised recommendations (Table 2)
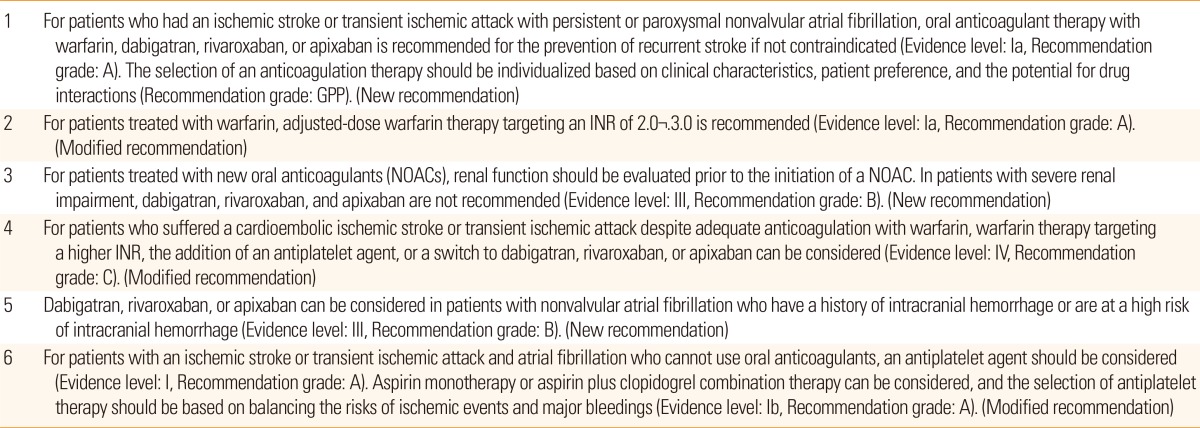
Guidelines for the antithrombotic management of patients with atrial fibrillation and ischemic stroke or transient ischemic attack
A full version of the updated proposal (in Korean) including detailed evidence is available in the Journal of the Korean Neurological Association.
For patients who had an ischemic stroke or transient ischemic attack with persistent or paroxysmal nonvalvular atrial fibrillation, oral anticoagulant therapy with warfarin, dabigatran, rivaroxaban, or apixaban is recommended for the prevention of recurrent stroke if not contraindicated (Evidence level: Ia, Recommendation grade: A). The selection of an anticoagulation therapy should be individualized based on clinical characteristics, patient preference, and the potential for drug interactions (Recommendation grade: GPP). (New recommendation)
The most notable change in the current revised guidelines is the recommendation of both NOACs and warfarin. The Ia evidence level for warfarin therapy in patients who suffered an ischemic stroke or transient ischemic attack with nonvalvular persistent or paroxysmal atrial fibrillation was assigned on the basis of the European Atrial Fibrillation Trial (EAFT) of warfarin for secondary stroke prevention7 and on an individual patient pooled analysis of 5 randomized controlled trials that included some secondary prevention subjects.8 For NOACs, large randomized controlled trials demonstrated that the efficacy and safety of dabigatran, rivaroxaban, apixaban, and edoxaban were at least non-inferior or superior to those of warfarin or aspirin.9,10,11,12,13,14 In subgroup analyses, the relative efficacy and safety of NOACs versus warfarin did not differ between patients with/without a prior history of stroke or transient ischemic attack.15,16,17,18 Moreover, the benefits of dabigatran were uniform across Asian and non-Asian subgroups.19 Despite the limitations inherent in combining heterogeneous trials testing different NOACs, 4 meta-analyses of overall trial populations and one meta-analysis that exclusively focused on patients with a prior history of stroke or transient ischemic attack consistently demonstrated that NOACs were superior to warfarin for stroke prevention as well as intracranial bleeding.20,21,22,23,24 While dabigatran, rivaroxaban, and apixaban were approved by the Korean Food and Drug Administration for stroke prevention in patients with nonvalvular atrial fibrillation, edoxaban has yet to be approved and was therefore excluded from this guideline statement. A Ia evidence level and A recommendation grade were assigned to NOACs for secondary stroke prevention in patients with atrial fibrillation. However, due to the lack of trials directly comparing NOACs, selection among the new anticoagulants was recommended at the GPP level to be dependent on patient characteristics including thrombosis risk, mechanism, comorbidities, patient preference, and the potential for drug interactions.
For patients treated with warfarin, adjusted-dose warfarin therapy targeting an INR of 2.0-3.0 is recommended (Evidence level: Ia, Recommendation grade: A). (Modified recommendation)
The Ia evidence level and A recommendation grade were assigned based on the EAFT treatment protocol targeting an INR of 2.0-3.07 and pooled data from 5 randomized controlled trials.8
For patients treated with NOACs, renal function should be evaluated prior to the initiation of a NOAC. In patients with severe renal impairment, dabigatran, rivaroxaban, and apixaban are not recommended (Evidence level: III, Recommendation grade: B). (New recommendation)
NOACs are mainly or partly eliminated by renal excretion. Therefore, renal function should be assessed prior to NOAC use. Renal dysfunction criteria for clinical trial enrollment are variable across different NOACs. The RE-LY9 and ROCKET-AF trials11 excluded patients with severe renal dysfunction (CrCl <30 mL/min), whereas the AVERROES12 and ARISTOTLE trials13 excluded patients with a serum Cr >2.5 mg/dL or CrCl <25 mL/min. In addition, regulatory approval for the use of NOACs in patients with renal dysfunction varies across countries. Taken together, these data indicate that NOACs should be selected very cautiously in cases of severely impaired renal function. This statement was given a III evidence level and B recommendation grade owing to the lack of well-designed studies.
For patients who suffered a cardioembolic ischemic stroke or transient ischemic attack despite adequate anticoagulation with warfarin, warfarin therapy targeting a higher INR, the addition of an antiplatelet agent, or a switch to dabigatran, rivaroxaban, or apixaban can be considered (Evidence level: IV, Recommendation grade: C). (Modified recommendation)
There are no validated data to serve as a basis for recommending antithrombotics for patients who had a cardioembolic ischemic stroke or transient ischemic attack despite adequate anticoagulation with warfarin. However, this is a scenario frequently encountered in clinical practice and we therefore provide a recommendation on the basis of expert consensus. For these patients, we recommend considering one of the following: a higher INR target, the addition of antiplatelet therapy, or a switch to dabigatran, rivaroxaban, or apixaban. The assigned evidence level and recommendation grade were IV and C, respectively.
Dabigatran, rivaroxaban, or apixaban can be considered in patients with nonvalvular atrial fibrillation who have a history of intracranial bleeding or are at a high risk of intracranial bleeding (Evidence level: III, Recommendation grade: B). (New recommendation)
No randomized controlled trials or experimental studies directly tested the efficacy and safety of any antithrombotic therapy for patients with nonvalvular atrial fibrillation who have a history of intracranial bleeding or are at a high risk of intracranial bleeding. However, a reduction of hemorrhagic stroke with dabigatran, rivaroxaban, and apixaban versus warfarin was demonstrated in randomized clinical trials9,10,11,12,13,14 and meta-analyses20,21,22,23,24 and further supported by subgroup analyses of patients with a history of stroke or transient ischemic attack.15,16,17,18
For patients with an ischemic stroke or transient ischemic attack and atrial fibrillation who cannot use oral anticoagulants, an antiplatelet agent should be considered (Evidence level: I, Recommendation grade: A). Aspirin monotherapy or aspirin plus clopidogrel combination therapy can be considered, and the selection of antiplatelet therapy should be based on balancing the risks of ischemic events and major bleedings (Evidence level: Ib, Recommendation grade: A). (Modified recommendation)
Although the efficacy of antiplatelet therapy is greatly inferior to that of anticoagulant therapy, a meta-analysis showed that compared with placebo, antiplatelet therapy significantly reduced the risk of stroke.25 Therefore, antiplatelet therapy is recommended for patients who cannot use oral anticoagulation therapy. The ACTIVE-A trial suggested that the addition of clopidogrel to aspirin was more effective than aspirin monotherapy, but increased the risk of major hemorrhage.26 Therefore, our recommendation is that combination therapy with aspirin and clopidogrel can be considered while balancing the risk of ischemic events and major bleedings in individual patients with a Ib evidence level and A recommendation grade.
Notes
This study was supported by a grant from the Korean Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A102065) and the Hallym University Specialization Fund (HRF-S-51).
The authors have no financial conflicts of interest.