Collateral Circulation in Ischemic Stroke: An Updated Review
Article information
Abstract
The collateral circulation plays a crucial role in maintaining perfusion to brain tissue in ischemic stroke, which prolongs the time window for effective therapies to be provided and ultimately avoids irreversible damage that may lead to worse clinical outcomes. The understanding of this complex vascular bypass system has advanced greatly in the past few years, yet effective treatments for its potentiation as a therapeutic target remain a challenge. The assessment of the collateral circulation is now part of the routine neuroimaging protocols for acute ischemic stroke, which provides a more complete pathophysiological picture in each patient that allows for a better selection for acute reperfusion therapies and a more accurate prognostication of outcomes, among other potential uses. In this review, we aim to provide a structured and updated approach to the collateral circulation while highlighting ongoing research areas with promising future clinical applications.
Introduction
Ischemic stroke is up to this day a leading cause of morbidity and mortality worldwide [1]. The presence of penumbra (i.e., potentially salvageable brain tissue that is at risk of progressing to infarct) is at the center of the rationale for providing acute reperfusion therapies, namely intravenous thrombolysis and endovascular procedures. Classically, the “time is brain” paradigm has been used and, accordingly, time windows for these treatments have been established. This concept emphasizes the idea that the faster the reperfusion is achieved, the higher the chances of preserving viable brain tissue will be, which ultimately improves functional outcomes. On the other hand, a later treatment might be futile because there is no significant volume of tissue to salvage and the chance of treatment-associated complications progressively increases with time. These concepts have been proven by sub-analyses of previous trials, which have shown a time-dependent benefit of acute reperfusion therapies even within the established time windows for treatment [2-5].
The widespread use of advanced neuroimaging has led to a better understanding of the dynamics of the progression of brain tissue from penumbra to infarct, to a better selection of patients for acute reperfusion therapies, and ultimately to the current ongoing expansion of the criteria to select patients for these treatments. The paradigm has accordingly been shifting from a time-oriented to a tissue-oriented approach. In this regard, the collateral circulation plays a critical role in sustaining viable brain tissue for longer periods and in allowing for reperfusion therapies to be given at later times. The “collateral clock” concept has accordingly been suggested [6]. Moreover, the collateral circulation can play several other roles in ischemic stroke and it has therefore emerged as a prognostic marker, a factor to consider when selecting patients for acute treatments, and a potential treatment target.
A deep understanding of the anatomy, physiology, pathophysiology, evaluation methods, clinical applications, and potential enhancement methods of the brain collateral circulation allows clinicians to provide better care for their patients with ischemic stroke and to contribute to the ever-growing knowledge in this field. In a previous review [7], these different aspects were analyzed; however, important advances in knowledge have been made during the past decade and, thus, we believe that an updated review is warranted.
Definition, anatomy, physiology, and factors that can affect the collateral circulation
The collateral circulation of the brain refers to alternative or indirect arterial pathways that can potentially provide blood flow when an artery that normally supplies an area of brain tissue is occluded (Table 1).
Anatomical classification of the collateral circulation
From a structural point of view, these pathways can be broadly divided into three anatomical categories (Figure 1).
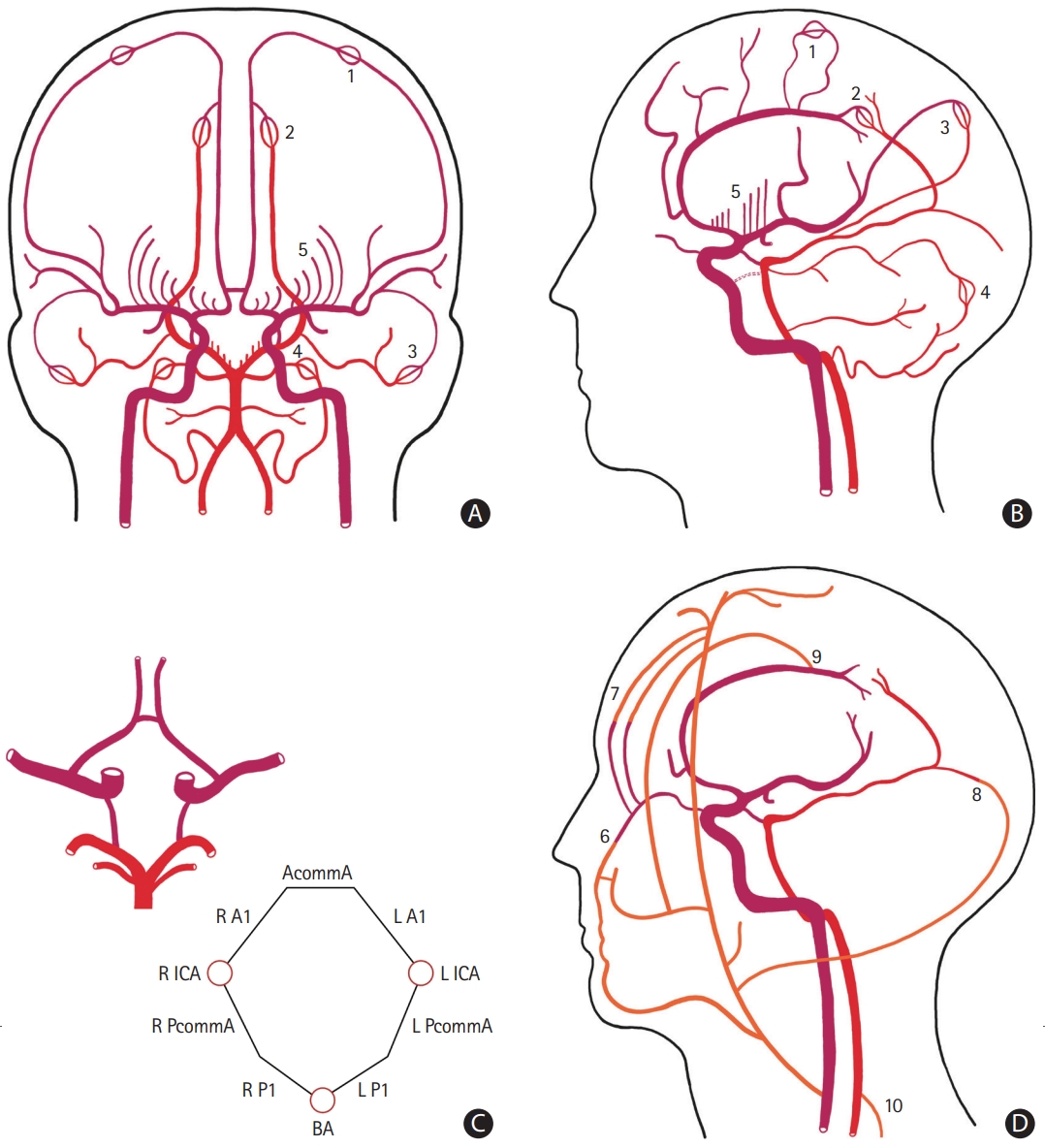
Schematic representation of the collateral circulation of the brain. The anterior circulation is represented in dark red, the posterior circulation in light red, and the extracranial sources of blood flow in orange. (A) Antero-posterior and (B) lateral view of the main intracranial arteries. The persistent carotid-vertebrobasilar anastomoses are represented with a dashed dark red line. (C) Inferior view of the circle of Willis and a corresponding diagram showing each arterial component. (D) Lateral view of cranio-cervical arteries highlighting the main extra-intracranial anastomoses. Microvascular anastomoses between (1) the anterior cerebral artery (ACA) and the middle cerebral artery (MCA), (2) the ACA and the posterior cerebral artery (PCA), (3) the MCA and the PCA, and (4) the superior cerebellar artery and the posterior inferior cerebellar artery. (5) The postulated collateral pathways in the deep subcortical territory. Extra-intracranial anastomoses between (6) branches of the facial artery and the ophthalmic artery, (7) the supraorbital and supratrochlear arteries and branches of the ophthalmic artery, (8) branches of the occipital artery and the PCA, (9) the middle meningeal artery and the ACA, and (10) branches from ascending and deep cervical arteries and the vertebral artery. AcommA, anterior communicating artery; R A1, A1 segment of the right ACA; L A1, A1 segment of the left ACA; R ICA, right internal carotid artery; L ICA, left internal carotid artery; R PcommA, right posterior communicating artery; L PcommA, left posterior communicating artery; R P1, P1 segment of the right PCA; L P1, P1 segment of the left PCA; BA, basilar artery.
Circle of Willis
The circle of Willis (CoW) is a ring of interconnected mediumsized arteries located at the base of the brain (Figure 1C). It connects the anterior and posterior circulations and the left and right hemispheres. The CoW can provide immediate diversion of blood flow in the case of an acute occlusion of a parent vessel. An important caveat is that the CoW has many possible variations and less than 50% of patients have a complete, symmetrical, and well-developed circle. These variations may significantly affect the capacity of the CoW to provide collateral pathways of blood flow and they have been shown to impact outcomes in ischemic stroke (Figure 2) [7,8].
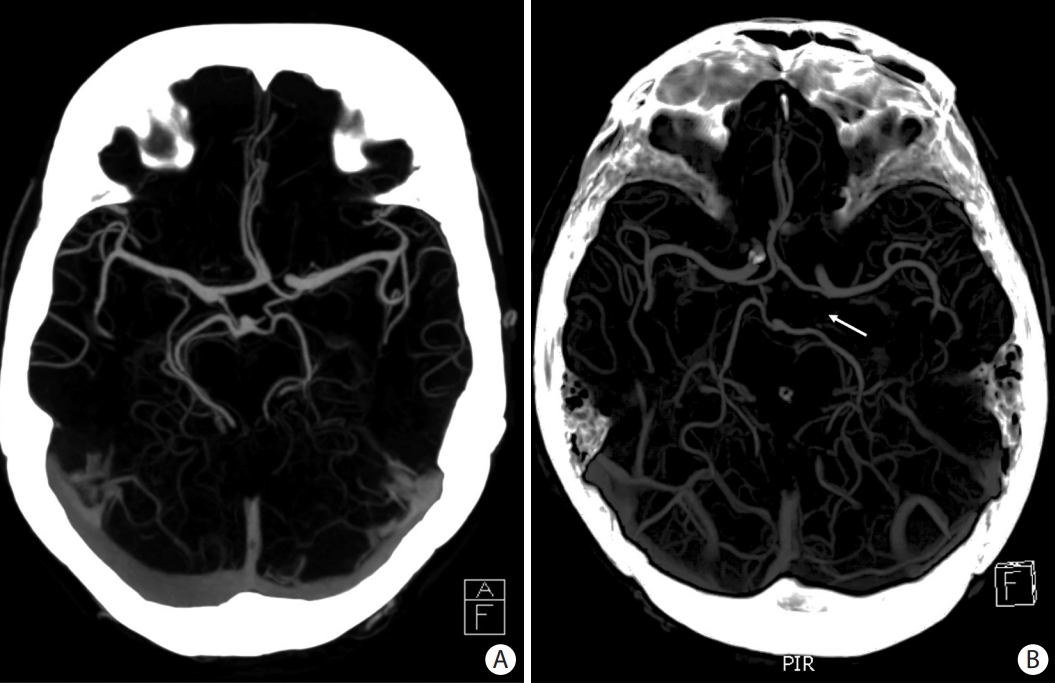
Axial maximum intensity projection computed tomography angiography slices showing examples of circle of Willis (CoW) configurations. (A) A complete CoW. (B) A CoW with absence of the left posterior communicating artery (arrow).
Carotid terminus occlusions are illustrative of the collateral potential of the CoW. These occlusions can take several forms (i.e., I-type, L-type, and T-type) with each having different patterns of collateralization [9]. The Willisian collateral status can also help predict outcomes in these patients [10].
Apart from the posterior communicating arteries, the persistent carotid-vertebrobasilar anastomoses are other possible connections between the anterior and posterior circulations. These arteries are present during the embryonic period and they usually involute, but they may rarely persist into adult life [8].
Microvascular intracranial collaterals
Leptomeningeal (pial) collaterals
These are small arteriolar connections (approximately 50–400 µm) at the distalmost branches of large cerebral and cerebellar vessels (Figure 1A and B). These connections display variable configurations including end-to-end and end-to-side anastomoses. Blood can flow in both directions through these anastomoses as a function of the hemodynamic and metabolic needs of the territories they connect [7].
If an occlusion of an intracranial vessel occurs, the leptomeningeal anastomoses can provide retrograde flow from the distal cortical areas of the territory of the occluded vessel (Figure 3).

Sequential antero-posterior images in digital subtraction angiography after contrast injection in the right internal carotid artery in a patient with an occlusion of the M1 segment of the right middle cerebral artery (arrow). Notice the contrast filling of the left anterior circulation through the anterior communicating artery (dashed arrow) in the earliest image. The direction of the blood flow through the leptomeningeal collaterals from anterior cerebral artery to middle cerebral artery is shown with a curved arrow.
The current available information shows that collateral formation and maturation is a complex process which involves several genes and pathways.
Collaterogenesis, or the formation of leptomeningeal collaterals, occurs during the embryonic period (Figure 4). Murine models have identified a locus on chromosome 7 whose allelic variants explain more than 80% of the variation in collateral extent. This locus has been called Determinant of collateral extent-1 (Dce1). The Rab GTPase-effector binding protein 2 (Rabep2) gene was subsequently identified as the causative allele at Dce1 [11]. Rabep2 is ubiquitously expressed and is involved in vascular endothelial growth factor-A (VEGF-A)/vascular endothelial growth factor receptor 2 (VEGFR2) signaling through vesicular trafficking [12]. Collateral formation is impaired in Rabep2-/- embryos. Mutations of Rabep2 do not affect pre- or postnatal development and growth of the general arterial-venous vasculature, capillary density, normal or tumor angiogenesis, or any other apparent phenotype other than collateral abundance [13]. Paracrine VEGF-A activates flk1 (VEGFR2) and initiates delta-like ligand 4 (Dll4) binding to Notch on adjacent endothelial cells. Dll4 is a transmembrane ligand of Notch receptors, selectively expressed in arterial and angiogenic tip cells during development. Its binding to Notch promotes a “tip cell” phenotype in an endothelial cell of a distal-most arteriole of the cerebral artery tree. A disintegrin and metalloprotease (ADAM) 10 and gamma-secretase cleavage activity are required for Notch intracellular domain (NCID) signaling and promotion of a “stalk cell” phenotype in the trailing endothelial cells. This endothelial sprouting process ultimately leads to the fusion of a terminal arteriole to an opposing arteriole, thus forming a new collateral [14,15]. Dll4-Notch signaling restricts pial collateral artery formation during embryogenesis. Dll4 heterozygous mice show an increased number of pial collaterals compared to littermates, but with no variation in the volume of infarcted tissue in middle cerebral artery (MCA) occlusion models and with no variation in outcomes in hindlimb ischemia models. These results suggest that not only the number of collaterals is important but also their functionality [16]. Apart from pathways involved in formation of pial collaterals, other pathways involved in their maturation have been studied. Chloride intracellular channel-4 (CLIC4) has a positive effect in collateral maturation while the endothelial-specific ephrin type-A receptor 4 (EphA4) has a suppressing effect on pial collateral remodeling [16,17]. Findings from murine models require further confirmation in humans.
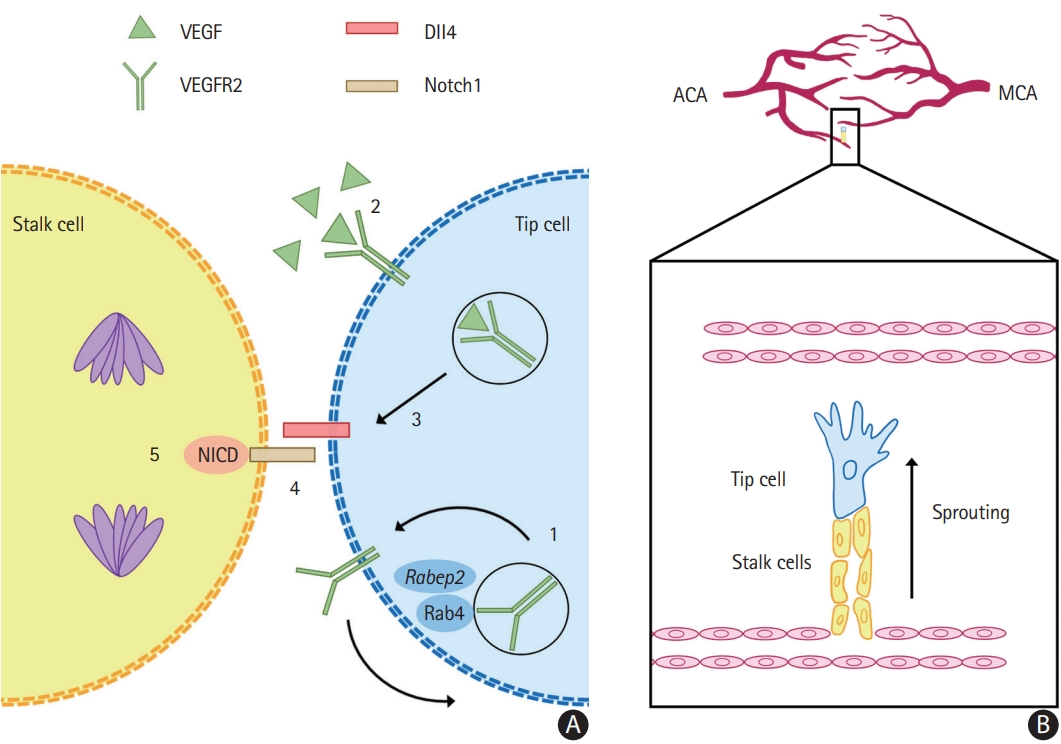
Collaterogenesis occurs during the embryonic period. (A) The differentiation of endothelial cells into tip and stalk phenotypes is dependent on vascular endothelial growth factor (VEGF)/vascular endothelial growth factor receptor 2 (VEGFR2) signaling. (1) Rabep2, whose genetic variations largely determine the differences on collateral extent in murine models, promotes the Rab4 recycling of VEGFR2 to the cell surface, increasing its availability. (2) VEGF binding to VEGFR2 induces endocytosis and signaling which (3) induces delta-like ligand 4 (Dll4). (4) Dll4 activates the transmembrane receptor Notch1, of which the Notch intracellular domain (NICD) is liberated and (5) induces several effects in the adjacent stalk cells, such as cell division. (B) Tip cells are guided by the VEGF gradient and direct the growing sprout while stalk cells follow behind and form the vascular lumen. This process leads to the fusion of two terminal arterioles, forming a new collateral. In the example, a new collateral is forming between terminal branches of the anterior cerebral artery (ACA) to middle cerebral artery (MCA). Rabep2, Rab GTPase-effector binding protein 2; Rab4, Rab GTPase 4.
Collateral circulation in small subcortical infarcts
The prevailing notion that small subcortical infarcts, with their different possible mechanisms, are caused by the occlusion of terminal penetrating arteries which lack collateral pathways has been challenged. There is evidence from post-mortem human studies of the presence of anastomoses between major perforator arteries and precapillary arterioles. Also, more recent studies using computed tomography (CT) and magnetic resonance (MR) perfusion techniques have provided indirect evidence of the presence of both anterograde and retrograde collaterals in small subcortical infarcts (Figure 1A and B). This suggests that the core-penumbra model may also be applied to this type of infarcts [18,19].
Extracranial sources of collateral circulation
There are several possible extra-intracranial anastomoses, which can provide blood flow in the case of a blood vessel occlusion. These extracranial sources originate from branches of the external carotid artery or from ascending and deep cervical arteries (Figure 1D) [7].
One example is an occlusion of the internal carotid artery (ICA) before the emergence of the ophthalmic artery. If there is a complete and functional CoW, the terminal ICA may receive retrograde flow through the circle and immediately restore the anterograde flow through the ophthalmic artery. If there is insufficient collateral circulation through the CoW, another possible source of blood flow are branches of the external carotid artery, which can anastomose with branches of the ophthalmic artery and provide retrograde flow, which will ultimately reach the terminal ICA [20].
Functional classification of the collateral circulation
From a functional point of view, the collateral circulation can be divided into primary, secondary, and tertiary types.
Primary
The primary collateral circulation corresponds to permanently functioning pathways that can immediately reroute blood flow when a blood vessel occlusion occurs. This term refers mainly to the CoW.
Secondary
The secondary collateral circulation refers to pre-existing arterial conduits that can instantaneously be recruited to provide an alternative pathway for blood flow. This refers mainly to the leptomeningeal collaterals. The recruitment of leptomeningeal collaterals is extremely fast. For example, in rat models of ICA occlusion, it takes only 12 seconds for leptomeningeal collaterals to reach their maximal vasodilatation [21].
There are several neurohumoral mechanisms involved in the process of leptomeningeal collateral recruitment. The main driver of the functionality of these pathways is pressure gradients [22]. It is important to keep in mind that in the context of an acute large vessel occlusion (LVO) the cerebral autoregulation is impaired and blood flow through collateral arteries becomes particularly dependent on the mean arterial pressure. In this sense, the resistance of the collateral network plays a determinant role. Shear stress through these vessels activates nitric oxide (NO)-dependent mechanisms that lead to their dilation and improved blood flow. There is also a neural regulation of the cerebrovascular tone through intrinsic (i.e., from the central nervous system) and extrinsic (i.e., from the peripheral nervous system) innervations. The intrinsic nerves originate mainly in the brainstem and are distributed predominantly in the parenchymal vessels, whereas the extrinsic nerves supply the vessels on the surface of the brain [23]. The extrinsic parasympathetic nerves, which arise from the superior salivatory nucleus and pass along cranial nerve VII to the sphenopalatine and otic ganglia, are involved in vasodilation and their stimulation has been studied as a therapeutic target. Several neurotransmitters are involved in these pathways, such as acetylcholine, vasoactive intestinal polypeptide, peptide histidine isoleucine and nitrous oxide [7].
Even though the extent and functionality of the collateral circulation in adulthood is largely determined by collaterogenesis and its implicated genes and pathways, it can also be modified throughout the patient’s life by several factors.
Age
Aging causes a decrease in number and diameter and an increase in tortuosity of leptomeningeal collaterals, which lead to increased vascular resistance. These changes are associated with impaired endothelial NO synthase (eNOS) signaling and increased oxidative stress. In a retrospective analysis of 70 patients with proximal MCA occlusion, every 10-year increment in age increased the odds of having poor collaterals by a factor of 1.87 (95% confidence interval [CI] 1.18–2.97) [24].
Vascular risk factors
These are frequent comorbidities in stroke patients and they may have negative effects on the collateral circulation. In animal models of chronic hypertension, induction of collateral flow during acute ischemic stroke is impaired. This is associated with highly vasoconstricted pial collaterals that respond to pressure myogenically [25]. Clinical studies have suggested that chronic hypertension has a detrimental effect on collateral flow in patients with LVO. This detrimental effect is highest in those with untreated hypertension and lowest in those without hypertension, while hypertensive patients treated with antihypertensive medications are in between [26]. Similarly, murine models of common carotid artery occlusion have shown impaired collateral flow in diabetic mice [27]. Previous reports from patients with coronary artery disease have suggested that smoking may be associated with better collaterals. The proposed mechanism is ischemic preconditioning; however, a 2021 meta-analysis of 18 studies and more than 4,000 patients did not demonstrate a positive association [28]. In the case of ischemic stroke, a retrospective analysis of embolic LVO in more than 600 patients found a positive correlation between smoking (current or previous) and good collaterals (odds ratio [OR] 1.74, CI 1.17–2.61, P=0.006) [29]. In a retrospective analysis of 206 consecutive patients with an M1 segment occlusion, multivariate analysis found the metabolic syndrome, hyperuricemia, and older age to be independent predictors of poor collaterals at baseline [30].
Physical exercise
Regular exercise has been shown to improve collateral circulation in patients with coronary artery disease and in animal models of stroke. Physical exercise increases blood flow and the shear stress stimulates different mechanisms in the endothelium, which lead to maintenance, defense, and repair of the vasculature. It also enhances the capacity of the vessels to vasodilate. Another more indirect effect of physical exercise is the reduction of vascular risk factors [31].
Statin use
Multiple observational studies have shown an association between previous statin use and better collaterals in ischemic stroke patients. Proposed mechanisms for this effect are enhancement of arteriogenesis and eNOS-mediated vasodilation. However, a 2019 meta-analysis of previous studies only showed a positive trend towards better collaterals. No differences between stroke subtypes were demonstrated [32].
Extracranial carotid stenosis
In an observational study of 385 patients who underwent mechanical thrombectomy for LVO, patients with an ipsilateral stenosis of the extracranial ICA of more than 75% had an OR of 4.01 for having good collaterals (95% CI 1.78–9.00; P=0.001) [33].
Tertiary
The term tertiary collaterals is sometimes used to refer to the formation of new blood vessels or the maturation of pre-existent vessels in ischemic areas [34]. Two main processes are involved. Angiogenesis is the physiologic process in which new blood vessels arise from pre-existent ones. The main stimuli for angiogenesis are ischemia and hypoxia. In contrast, arteriogenesis refers to the maturation of pre-existent arterioles into arteries. It is an important process of adaptation of blood vessels to new demands from tissue at risk after an arterial occlusion. The main stimulus for arteriogenesis is the shear stress on the endothelium, which is generated by pressure gradients [35]. These processes take a longer time to develop, and thus their role is mainly in the context of chronic vascular occlusions. An illustrative example of tertiary collaterals is the moyamoya vessels that develop in patients with moyamoya disease and syndrome.
The role of the collateral circulation in ischemic stroke
The main role of the collateral circulation is to maintain blood flow to the tissue that is normally supplied by an occluded vessel. This slows down the progression of tissue from penumbra to infarct, thus increasing the therapeutic time window, decreasing the final stroke volume, and decreasing the risk of hemorrhagic transformation [36]. The rate of progression from penumbra to infarct greatly depends on the extent of the collateral circulation and ultimately determines whether the patient will be a fast or a slow progressor. The persistence of blood flow to the blood clot also enhances the delivery of endogenous or exogenous tissue plasminogen activator, which increases the recanalization rate and decreases the re-occlusion rate. Likewise, in the case that potential neuroprotective agents are used, the collateral circulation can also enhance their delivery to brain tissue.
A functional venous drainage system is also important in ischemic stroke and it can enhance the function of the arterial collaterals. The possible roles of the venous system in this context can be broadly divided into the maintenance of sufficient collateral perfusion via adequate drainage of blood and clearance of microemboli, and the reduction of reperfusion injury [37].
Evaluation of the collateral circulation
The methods to assess the collateral circulation can be broadly divided into structural and functional types; however, there may be overlap in the type of information that they can provide.
Structural studies
These are imaging studies that visualize blood vessels and give an insight of the status of the collateral circulation either by static or dynamic acquisitions, but the actual anatomical connections are not necessarily seen.
Digital subtraction angiography
Digital subtraction angiography (DSA) is considered the gold standard for structural assessment of the collateral circulation. This technique allows for the dynamic evaluation of blood flow with an excellent spatial and temporal resolution. It allows the assessment of the three main anatomical collateral pathways: the CoW, the extra-intracranial anastomoses, and the leptomeningeal collaterals. Its main disadvantages are its invasive nature, its associated procedural risks, the need for contrast agent administration, and its limited availability.
Methods based on CT
These are the most frequently used studies in the assessment of the collateral circulation because of their widespread availability and the brief additional time needed to perform them.
Single-phase CT angiography (sCTA), which is performed at a single time point in relation to the contrast bolus injection, has the limitation of being a static evaluation and can therefore provide an inexact measurement of the state of collaterals if the acquisition is not performed at the optimal time point. For example, in patients with a diminished cardiac ejection fraction or an extracranial carotid stenosis, the collaterals may be underestimated because the image acquisition will tend to be performed before the contrast agent can reach the leptomeningeal vessels. Previous studies have suggested that collateral assessment in sCTA in the early arterial and late venous phases underestimate and overestimate the collateral status, respectively. Probably the optimal timing for collateral grading on sCTA is in the peak arterial to equilibrium phase [38]. The collateral filling distal to a vascular occlusion may be better visualized on post-processed maximum intensity projection images [39].
Multiphase CTA (mCTA) is performed in different time points and provides a better characterization of the collateral circulation than sCTA because it allows the assessment of the delay in contrast arrival and washout. This technique also has a better interrater reliability for the detection of LVO, it allows for a more precise assessment of the thrombus length, and it has a better association with final infarct volume and clinical outcomes. mCTA requires brief extra time to be performed and it does not require additional contrast injection when compared to sCTA. At our institution, we routinely perform mCTA in three time points and rate the collaterals as described by Menon et al. [40] (Figure 5).
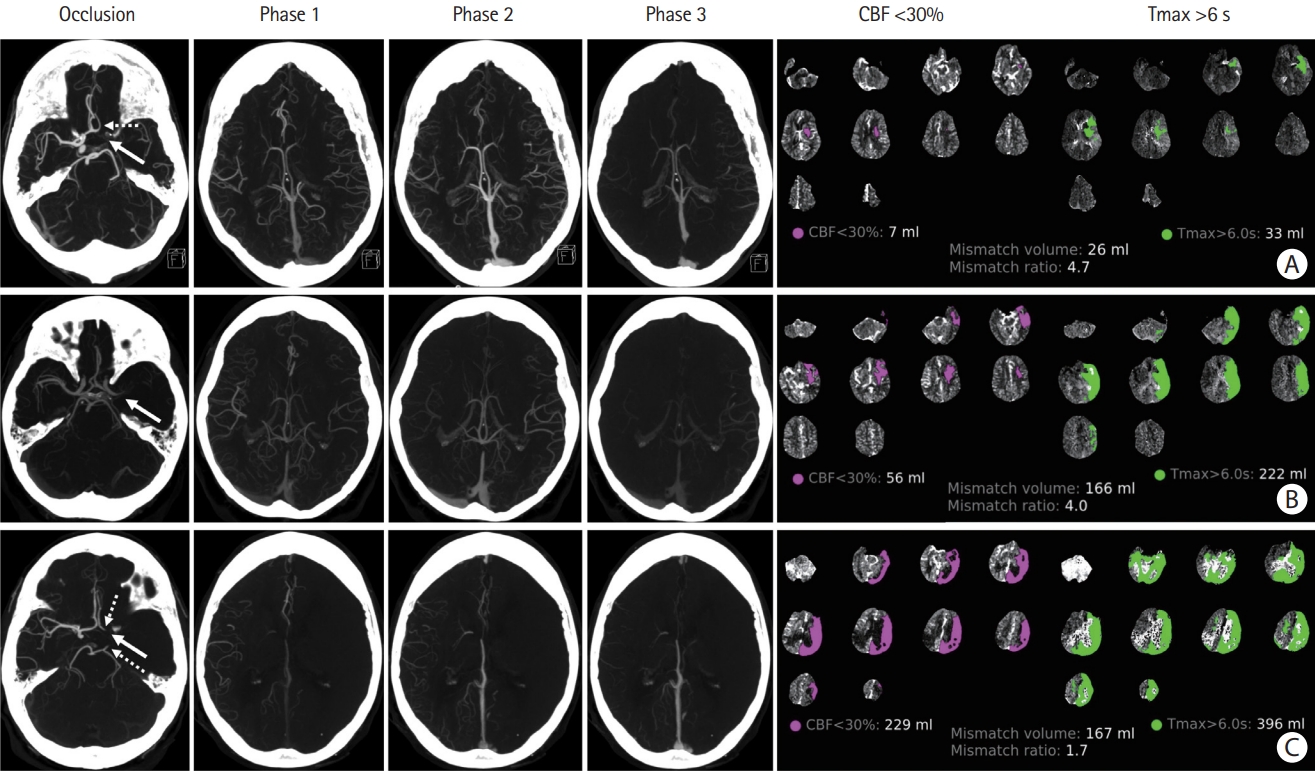
Examples of patients with acute large vessel occlusion (LVO) and their respective computed tomography agiography (CTA) and computed tomography perfusion studies. Each row sequentially shows axial maximum intensity projection images of the LVO and the three phases of CTA, followed by the ischemic core (defined as cerebral blood flow [CBF] <30% of contralateral side) and penumbra (defined as time-to-maximum [Tmax] >6 s) images with their respective automated volume calculation. (A) Left “T occlusion” (distal internal carotid artery, A1 and M1 segments, arrow) with good collaterals. Notice the filling of the left A2 segment from the contralateral side (dashed arrow). (B) Left M1 occlusion (arrow) with moderate collaterals. (C) Left “T occlusion” (arrow) with poor collaterals. Notice the retrograde filling of the left A1 segment and left posterior communicating artery (dashed arrows).
Methods based on MR
These techniques have well-known advantages over CT-based methods but they are not as readily available and they are usually slower to perform. However, advances in hardware and the development of novel imaging techniques have decreased acquisition times and thus MR-based protocols for acute imaging of stroke are becoming more commonly used [41].
Time-of-flight MR angiography (TOF-MRA) is a T1-based sequence that does not require gadolinium injection and is used to assess the proximal intracranial vasculature. It is based on blood flow which generates a visible signal. Its disadvantages are the acquisition time (approximately 5 minutes) and poor resolution of distal vessels. Also, slow flow distal to the occlusion can generate a complete loss of signal, which leads to an overestimation of the areas of occlusion. A significant advantage of TOF-MRA is that it can easily be reformatted into three-dimensional images because of its volumetric acquisition method [39].
Contrast-enhanced MR angiography (CE-MRA) is also a T1-based sequence and it requires the injection of a bolus of gadolinium. Its advantages are a high signal-to-noise ratio and a relative insensitivity to slow flow [42].
The fluid-attenuated inversion recovery (FLAIR) sequence can also provide information about collateral circulation. Vascular hyperintensities represent a more indirect marker of leptomeningeal collaterals, but they are non-specific and their usefulness is limited. The location of these hyperintensities in relation to the ischemic area is probably associated with the cerebral hemodynamic status. It has been observed that patients who have vascular hyperintensities only inside the ischemic area have worse collaterals when compared to patients who have vascular hyperintensities outside the ischemic area [43]. In a systematic review and meta-analysis of patients with ischemic strokes, FLAIR vascular hyperintensities as a whole were not associated with functional outcomes but an association was demonstrated for the subgroups of patients who underwent endovascular treatment and for those who had hyperintensities outside the ischemic territory [44].
Transcranial Doppler
This non-invasive method provides real-time information about intracranial blood flow. It only allows the assessment of proximal blood vessels at the level of the CoW, and it is an operator-dependent method. One possible finding is the inversion of blood flow through the ophthalmic artery or the A1 segment of the anterior cerebral artery (ACA) in the context of an ipsilateral distal ICA occlusion. Another possible finding is the flow diversion phenomenon, which refers to the findings of high velocity and low resistance in the ipsilateral ACA and/or posterior cerebral artery (PCA) in the context of an MCA occlusion. This is associated with the presence of anastomoses between the distal branches of the ACA/PCA and the MCA. These findings have shown a sensitivity of 81% and a specificity of 76% when compared with DSA for the presence of leptomeningeal collaterals [45].
Functional studies
Tissue perfusion studies allow for the assessment of the compensation by the collateral circulation.
CT perfusion
CT perfusion (CTP) is widely available, fast, and together with non-contrast CT and CTA is a part of the multimodal acute stroke neuroimaging protocol in many centers, including ours (Figure 5). In this technique, multiple acquisitions of the brain parenchyma are performed during contrast infusion. As the contrast flows through the brain, the increase, peak and decrease of density are captured in a time-density curve, which allows for the calculation of different perfusion parameters [39]. In particular, the volume of ischemic core and penumbra can be calculated using standardized definitions. These measurements are routinely used to select patients for acute reperfusion therapies.
Different softwares may be employed for the processing of perfusion images, such as the rapid processing of perfusion and diffusion (RAPID) software (IschemaView, Menlo Park, CA, USA) which is routinely used at our center and which also employs artificial intelligence (AI) technology to detect LVOs. CTP studies usually require an additional dose of contrast agent. Interestingly, the StrokeSENS™ software (Circle Neurovascular Imaging, Calgary, AB, Canada) allows perfusion studies to be performed from mCTA images without the need of an additional dose of contrast agent and it can also perform AI-based automated Alberta Stroke Program Early CT Score (ASPECTS) scoring from non-contrast CT images and LVO detection from CTA images. This software is available for clinical use in the EU, UK, Canada, Australia, and USA but only for LVO detection, with the rest of the features currently reserved for research purposes [46]. There are several other AI-based softwares that can perform automated interpretation of neuroimaging in acute stroke [47].
CTP can also be helpful in estimating the rate of progression from penumbra to ischemic core and thus in differentiating between fast and slow progressors, which can have implications in management and prognosis of acute stroke patients with LVO. The hypoperfusion index (HI) was first described in 2008 and is now preferably calculated as the ratio of time-to-peak concentration at >10 seconds divided by time-to-peak concentration at >6 seconds. In a cohort of medium-vessel-occlusion and LVO patients, an HI >0.5 versus ≤0.5 accurately differentiated fast from slow progressors, respectively, in the first 24 hours of an ischemic stroke (Figure 6) [48].
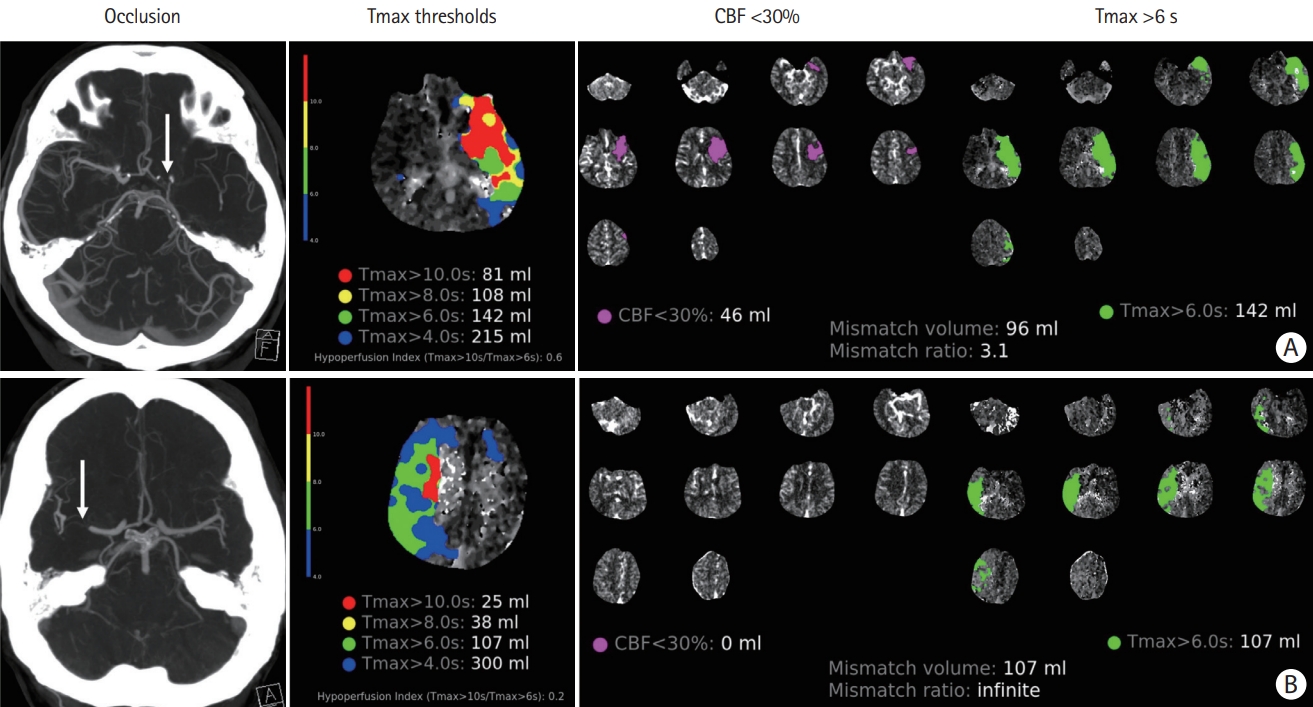
The hypoperfusion index (HI=Tmax>10 s/Tmax>6 s) in fast versus slow progressors. (A) Fast progressor: patient with an acute left “L occlusion” (distal internal carotid artery extending into the middle cerebral artery [MCA], arrow) with imaging performed 90 minutes after onset of symptoms. HI=0.6. (B) Slow progressor: patient with an acute right MCA occlusion (arrow) with imaging performed 120 minutes after onset of symptoms. HI=0.2. CBF, cerebral blood flow.
There are several possible clinical situations that may produce false positive and false negative results in CTP studies, so their results should always be interpreted considering the clinical picture and the concomitant vascular imaging. Some examples of these situations are migraine aura, seizures, and large vessel stenosis which can alter the local hemodynamic balance.
MR perfusion
Similar to CTP, in MR perfusion-weighted imaging (PWI), the signal intensity of the brain is measured at different intervals while a contrast agent is administered intravenously. Perfusion parameters can be calculated from the time-concentration curve after deconvolution [49]. However, in the case of MR-based studies, the infarct core is most accurately estimated not by perfusion parameters but by diffusion-weighted imaging (DWI), which shows areas of cytotoxic edema only minutes after the onset of ischemia. DWI is more sensitive for the detection of acute ischemia than CT-based methods, especially for small subcortical infarcts. DWI-PWI mismatch is routinely used in MR-based studies to determine the area of penumbra [50,51].
Positron emission tomography CT and single-photon emission CT
Tissue perfusion studies can also be performed with positron emission tomography CT and single-photon emission CT, but these are mostly reserved for investigation purposes. They can be combined with a vasodilator stimulus, such as in the acetazolamide challenge test, to assess the cerebrovascular reserve in a given patient [52].
Other methods to assess the collateral circulation
Arterial spin labeling (ASL) is an MR-based technique that provides a quantitative measurement of cerebral blood flow (CBF) and it has the advantage of not requiring the administration of a contrast agent. It can also provide structural information of pial collaterals, which can be visualized as linear hyperintense regions of increased CBF in the periphery of the area of ischemic penumbra. Despite its advantages, ASL has not gained widespread use in stroke for several reasons, most importantly for its high sensitivity to differences in arterial arrival time which may ultimately lead to an overestimation of CBF and an underestimation of tissue at risk. These shortcomings might be mitigated by methodological improvements [53,54]. The presence of collaterals detected by ASL are correlated with good clinical outcomes in retrospective series of patients with acute ischemic stroke. The Imaging Collaterals in Acute Stroke (iCAS) is an ongoing prospective cohort study of patients undergoing ASL imaging before mechanical thrombectomy and it is evaluating the relationship between pre-treatment collateral status and response to thrombectomy and functional outcomes [39]. This information might be valuable for the potential addition of ASL into MR-based imaging protocols in acute ischemic stroke.
The methods to assess the collateral circulation that we have mentioned so far imply the presence of a large vessel stenosis or occlusion that ultimately causes the pial collateral channels to be open (i.e., to be recruited). However, having a non-invasive imaging biomarker of the collateral status before a vessel occlusion or stroke occurs is a current need because it would provide valuable information for understanding the physiology and pathophysiology of the collateral circulation during a patient’s life, it could serve as a prognostic marker, and it would also help evaluate potential early therapeutic strategies of collateral circulation augmentation.
Retinal vessel metrics have been proposed as a surrogate marker of leptomeningeal collateral status. Retinal fundus images have previously been used to identify alterations in the retinal vasculature to predict stroke and it has been observed that retinal vessel width differs between stroke subtypes and between patients with recurrent strokes. Murine models of acute ischemic stroke have identified several retinal vessel parameters that predict the pial collateral status, infarct volume, and neurological outcomes. A recent translational human study showed that standard retinal vessel metrics such as venular widening and lower arterio-venular ratio and tortuosity differ in patients with acute ischemic stroke when compared to healthy controls, but they do not differentiate patients with good from those with poor pial collaterals. On the other hand, increased retinal vessel multifractal dimensions were shown to be a marker of poor pial collaterals in patients with acute ischemic stroke. These findings need to be confirmed on larger studies, and the usefulness of these metrics in patients with intra- or extracranial vascular stenosis or occlusion prior to ischemic stroke remains to be explored [55].
Scales used in the assessment of the collateral circulation
Numerous scales have been created to standardize the evaluation of the collateral circulation. They are based on the different available study methods and use different criteria to grade the extent of collaterals [39]. Several of them dichotomize the grading into good and poor collaterals. The variable use of these different scales can make it difficult to compare studies regarding the collateral circulation and its different possible clinical uses. Moreover, the concordance between different modalities has been shown to be poor [56]. A recent pooled analysis of patient-level data from the Highly Effective Reperfusion evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration comparing three different collateral scales showed that a regional collateral scale on sCTA provided the most accurate prediction of functional outcome, while on time-resolved CTA there were no differences among the different scales [38]. Automated methods based on AI are promising techniques to improve and standardize the evaluation of the collateral circulation; however, their use is currently only approved for investigational purposes [47].
Given the importance of a functional venous drainage system and its complementary and synergistic nature with the arterial collateral system in the context of acute ischemic stroke, scales that grade the venous drainage either by itself or in combination with an arterial collateral grading system have been devised. Several of these scales have shown a significant association with outcomes and complications such as hemorrhagic transformation [57-61]. These findings suggest that venous collateral grading might be used as an additional imaging biomarker for outcome prediction and possibly treatment selection in acute stroke patients.
Clinical applications
The collateral status might provide insights into the etiology of LVOs
Intracranial atherosclerotic disease (ICAD) is a major etiology of stroke, especially in patients of certain ethnicities. ICAD can cause strokes by several mechanisms, one of them being hypoperfusion secondary to progressive stenosis. In such cases, the longstanding ischemia may lead to the progressive recruitment or development of collaterals as opposed to an acute embolic occlusion [62]. In line with these pathophysiological mechanisms, previous studies have reported a possible role of collateral status observation either by structural or functional methods in determining the etiology of stroke [63-65]. A recent meta-analysis in patients with acute stroke receiving reperfusion therapies found that large artery atherosclerosis etiology was associated with a significantly increased rate of pre-treatment good collaterals (risk ratio [RR] 1.24; 95% CI 1.04–1.50; P=0.020) when compared to cardioembolic etiology, but with heterogeneity between studies [66].
The collateral circulation is a prognostic factor for both clinical and imaging outcomes in ischemic stroke
Overall prognosis
Poor collaterals on admission are associated with a larger ischemic core and worse clinical outcomes [67]. In the first 48 hours of an ischemic stroke, the presence of good collaterals is associated with early clinical improvement. Patients with poor collaterals have higher frequency of hemorrhagic transformation, both symptomatic and asymptomatic [68]. In a large prospective cohort of patients with LVO, the presence of good collaterals was an independent predictor of good long-term outcomes, and this effect was more evident if they did not receive reperfusion therapies. In a large cohort of patients with LVO and multimodal CT imaging, it was noted that the collateral status is not consistently associated with the size of the penumbra, but it is associated with the core volume and its growth speed [69,70].
In the case of ICAD, the association of good collaterals with better outcomes may not be valid because in these cases the occurrence of a stroke might represent an exhaustion of the collateral system. However, there is scarce data to support this notion and more information is needed [60]. In a retrospective analysis of the Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) trial the quality of collaterals independently predicted the occurrence of new strokes in the symptomatic territory [71].
Prognosis in intravenous thrombolysis
In a systematic review and meta-analysis which included 25 retrospective cohorts and 3 post-hoc analyses of randomized controlled trials (RCTs) and a total of 3,057 patients, those with good collaterals had a lower risk of symptomatic hemorrhagic transformation (RR 0.38; 95% CI 0.16–0.90; P=0.03), a higher frequency of early neurological improvement (RR 4.21; 95% CI 1.57–11.28, P=0.004), a higher frequency of good clinical outcomes (modified Rankin Scale [mRS] 0–2) at 3–6 months (RR 2.45; 95% CI 1.94–3.09; P<0.001), a lower National Institutes of Health Stroke Scale (NIHSS) on admission (median difference of 6 points), and a smaller infarct volume on admission. There were no statistically significant results associated with collateral status for successful recanalization and reperfusion, global risk of hemorrhagic transformation, final infarct volume, and mortality at 3 months [72].
Prognosis in endovascular thrombectomy
In two systematic reviews and meta-analyses which included studies that were published until March 2015, good collaterals before the endovascular procedure were significantly associated with a higher frequency of successful reperfusion as measured by the modified Thrombolysis in Cerebral Infarction (mTICI) score (RR=1.28; 95% CI 1.17–1.40; P<0.001), a higher frequency of successful recanalization as measured by the Arterial Occlusive Lesion (AOL) score (RR=1.23; 95% CI 1.06–1.42; P=0.006), a higher frequency of good funcional outcome (mRS≤2) at 90 days (RR=1.98, 95% CI 1.64 to 2.38; P<0.001), a reduced risk of periprocedural symptomatic intracranial hemorrhage (sICH) (RR=0.59; 95% CI 0.43 to 0.81; P=0.001) and death at 90 days (RR=0.49; 95% CI 0.38 to 0.63; P<0.001) [73,74]. Table 2 shows studies published after March 2015 that reported the association of collateral status and outcomes in patients treated with endovascular thrombectomy (EVT) for anterior circulation LVO stroke [40,75-92]. A similar analysis for vertebrobasilar LVO can be found in a recent review, showing conflicting results [93].

Selected studies reporting the association between pre-treatment collateral status and outcomes after EVT of anterior circulation large vessel occlusion stroke
When considering specifically patients in the late time window (6–24 hours since symptom onset), better collaterals are significantly associated with smaller CTP core, smaller penumbra, larger mismatch ratio, lower HI, and better functional outcomes [92,94].
The collateral circulation has become an important factor to consider when selecting or excluding patients from acute reperfusion therapies
The latest American Heart Association/American Stroke Association guidelines suggest that it may be reasonable to incorporate collateral flow status into clinical decision-making in some candidates to determine eligibility for mechanical thrombectomy with a IIb level of evidence. No specific criteria are suggested [95].
Considering the overall ominous functional prognosis in patients with pre-procedure poor collaterals, one may make a case for excluding these patients from EVT. However, it must be kept in mind that the number of patients in previous analyses was small and that probably the collateral status is one more of several factors that should be considered when making such a decision [79].
We may highlight some special groups of patients when considering the collateral status as a factor to select or exclude patients from acute reperfusion therapies.
Patients with low ASPECTS
There are several ongoing trials to assess the effectiveness and safety of EVT in patients with a low baseline ASPECTS. The collateral status may be an important factor to consider when selecting these patients. In a retrospective analysis of 100 patients with LVO and ASPECTS ≤5 who were treated with EVT, a good collateral status and younger age (<73 years) were associated with better functional outcomes [96].
Patients presenting in the late time window (6–24 hours from symptom onset) and very late time window (>24 hours from symptom onset)
A pooled analysis of late window EVT studies compared patients selected using collateral status plus perfusion imaging (current standard criteria) with those selected using collateral status only. They found no significant difference in functional outcomes at 3 months, but sICH was twice more frequent in the collateral only group with no significant difference in mortality at 3 months [97]. There are currently two ongoing trials evaluating patient selection for late window EVT with CT and CTA which could provide more insight into this issue: Randomization of Endovascular Treatment in Acute Ischemic Stroke in the Extended Time Window (RESILIENTExt, NCT04256096; Brazil) and Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands for Late Arrivals (MR CLEAN-LATE, ISRCTN19922220; Netherlands). Such approaches that do not require CTP might help us expand the access to EVT.
There is limited data evaluating the safety and efficacy of very late window EVT, but well-selected patients might benefit from this treatment, highlighting the importance of a tissue-based approach rather than a time-based approach to acute reperfusion therapies. A trial to assess EVT beyond 24 hours will probably require a collaborative approach from multiple centers given the low number of patients that might be eligible [98-100]. Assessment of the collateral circulation might also be an important factor to consider when selecting these patients.
The collateral circulation is an important factor to consider when determining the optimal blood pressure level in the peri-EVT period
The optimal blood pressure (BP) management strategy in the peri-EVT period is an ongoing area of research. Enhancing the collateral perfusion before recanalization and avoiding reperfusion damage and hemorrhagic transformation after recanalization are of utmost importance to achieve better functional outcomes. Patients with better collaterals might have better tolerance to BP fluctuations and it has been shown that poor baseline collaterals can aggravate the deleterious effects of higher BP levels or higher BP variability on clinical outcomes [101].
The collateral circulation is an important factor to consider when evaluating experimental neuroprotective agents
The Efficacy Study of Combined Treatment With Uric Acid and rtPA in Acute Ischemic Stroke (URICO-ICTUS) trial was an RCT in patients treated with intravenous thrombolysis to assess the administration of uric acid before the thrombolytic infusion was completed. The trial was negative for the primary outcome of better functional outcome at 3 months. In a posterior nested study that divided the patients by collateral status, only those with excellent collaterals had significantly better functional outcomes after the administration of uric acid. This example emphasizes the possible role of collaterals in the delivery of potential neuroprotective agents to the ischemic tissue [102].
Therapeutic strategies
Several treatment options to enhance the collateral circulation have previously been tested in clinical trials. Currently, none of these strategies have demonstrated a clear benefit to recommend their regular use. However, several of them have had promising results, and there are ongoing trials trying to prove their benefit.
Extracranial-intracranial indirect bypass surgery
The management of ICAD can be challenging, especially when best medical therapy fails. The use of invasive procedures in this situation raises the concern for associated adverse events.
Encephaloduroarteriosynangiosis (EDAS) is an indirect extracranial-intracranial (EC-IC) bypass surgical technique, which is most described as a treatment option for patients with moyamoya disease/syndrome. The EDAS Revascularization for Symptomatic Intracranial Atherosclerotic Steno-occlusive (ERSIAS) trial was a phase-II single-arm trial in patients with symptomatic ICAD (>70% stenosis in the intracranial ICA or M1 segment) and failure to best medical therapy. It compared EDAS plus intensive medical therapy versus intensive medical therapy alone. They found a reduction of any stroke or death in the first 30 days or any stroke in the territory of the affected vessel thereafter, reaching the non-futility threshold for advancement to a phase-III trial, with only mild surgical complications and no ICH. A post-hoc analysis of the trial, which only considered patients with borderzone infarcts, which are considered to have a higher risk of recurrence, found a significant reduction of the primary endpoint. A phase-III trial is expected [103].
Remote ischemic conditioning
Ischemic conditioning is a technique that consists of producing transient ischemia—but not necrosis—in a tissue. It can be performed directly, e.g., on a coronary artery, or remotely, e.g., on a limb. It is believed that it activates endogenous protective pathways in distant organs such as the kidney, the heart, and the brain via humoral, immune, and neural mechanisms [104]. Remote ischemic conditioning (RIC) can be applied as preconditioning (i.e., before the ischemic event), perconditioning (e.g., during the ischemic event), or postconditioning (i.e., after the ischemic event).
RIC has been evaluated in acute myocardial infarction, where it has demonstrated a reduction in infarcted tissue in ST-segment elevation myocardial infarction patients, but with no benefit in clinical outcomes [105]. In the case of ischemic stroke, clinical studies have not revealed a clear benefit to recommend its use. There is low-quality evidence suggesting that postconditioning might have a beneficial effect on clinical and neuroimaging outcomes [106,107]. There are several ongoing trials of RIC in acute ischemic stroke [105,108,109].
RIC is a simple, low-cost, and safe treatment, so the demonstration of its benefit could easily lead to widespread implementation.
Sphenopalatine ganglion stimulation
As we mentioned before, the stimulation of the extrinsic parasympathetic pathway has an effect on the intracranial vasculature. Specifically, pre-clinical and physiological studies have determined at least four mechanisms by which the stimulation of the sphenopalatine ganglion (SPG), a parasympathetic ganglion located in the pterygopalatine fossa, could be beneficial in ischemic stroke: vasodilation with the subsequent increase in blood flow through collateral pathways, stabilization of the bloodbrain barrier, neuroprotection via central cholinergic and adrenergic pathways, and enhancement of neuroplasticity [110].
The stimulation of the SPG through an implantable device has been tested in the injectable implant to stimulate the sphenopalatine ganglion for treatment of acute ischaemic stroke (ImpACT) trials, but they failed to show a significant benefit in the intention to treat population. However, they did demonstrate a significant benefit as an improvement beyond expectation in the mRS in the subgroup of patients with a confirmed cortical infarct, highlighting the importance of adequate patient selection [111].
Capsaicin (8-methyl-N-vanillyl-trans-6-nonenamide)—a component of hot chili peppers—is being investigated as a non-invasive alternative for the stimulation of the SPG. In a pilot study performed in healthy volunteers, oral capsaicin showed a dose-dependent augmentation of the MCA mean velocity and diminution of the pulsatility index on transcranial Doppler [112].
NO donors
NO donors are candidate neuroprotective agents in acute ischemic stroke. Due to their vasodilator effects, they are postulated to produce a potentiation of collateral circulation and a decrease in blood pressure. Nitroglycerin is a systemic NO donor and vasodilator. Its transdermal administration has been tested in the context of acute ischemic and hemorrhagic stroke, but no clinical benefit has been demonstrated when given within 6 hours of symptom onset [113]. It has been suggested that an earlier administration of nitroglycerin may provide clinical benefit; however, recently the prehospital transdermal glyceryl trinitrate in patients with presumed acute stroke (Multicenter Randomized trial of Acute Stroke treatment in the Ambulance with a nitroglycerin Patch [MR ASAP]) trial failed to demonstrate a clinical benefit of this treatment when applied within 3 hours of symptom onset in the prehospital setting. Interestingly, the study suggested a possible harm in ICH patients, in whom we might have suspected that the BP lowering effects would have been beneficial [114].
Other vasodilator agents
PP-007 (previously Sanguinate™, SG) is a PEGylated carboxyhemoglobin (PEG-COHb) gas transfer agent with pleiotropic effects on the brain and cerebral circulation. Its protective effects are thought to be mediated by several mechanisms, including vasodilation. Preclinical studies have demonstrated decreased neurological deficits, reduced infarct volume, and collateral enhancing properties of SG. There is an ongoing phase 1 multicenter clinical trial for treatment of LVO in patients undergoing endovascular thrombectomy (Safety Study of PP-007 in Subjects With Acute Ischemic Stroke [HEMERA-1]) [25].
Rapamycin is an inhibitor of mammalian target of rapamycin, which has been shown to be neuroprotective in animal models of stroke. In a rat model of stroke, rapamycin increased collateral perfusion during MCA occlusion and reperfusion. The observed dilation of leptomeningeal anastomoses was abolished by NOS inhibition, suggesting NO release as a mechanism of collateral enhancement by rapamycin. Currently, no clinical trials of rapamycin in acute ischemic stroke are ongoing [25,115].
TM5441 is a selective inhibitor of plasminogen activator inhibitor-1. It has a vasodilator effect that is mediated through NO release. In a rat model of stroke, the infusion of TM5441 increased collateral perfusion and reduced early infarct. Currently, no clinical trials of TM5441 in acute ischemic stroke are ongoing [25,116].
Conclusions and future challenges
Significant advances in the field of brain collateral circulation research have been made in the past few years. Our understanding of this complex bypass system during all stages of life in both healthy and morbid states is ever-growing, yet still incomplete. There is robust evidence to support the idea that the collateral circulation is a major determinant of outcomes in ischemic stroke and thus effective strategies to potentiate it are a current necessity.
Early interventions to potentiate the collateral circulation and avoid its rarefaction with age and other comorbid factors may have a significant impact in patients with acute stroke. In this regard, a deeper understanding of collaterogenesis and the factors that impact the collateral circulation across a patient’s life might reveal new potential intervention strategies. Assessment methods of the collateral circulation before a stroke occurs are also a necessity in the development and evaluation of these early intervention strategies.
More comprehensive scales that consider not only the arterial bypass routes but also the importance of the venous drainage system, and also a standardization of assessment methods is needed to better assess this complex system and to simplify communication and collaboration in research and daily clinical practice. Automated AI-based softwares are a promising tool for this purpose.
Safe and effective methods for acute potentiation of the collateral circulation in the context of acute ischemic stroke are also important, given that this will most likely remain the most common situation in which we might potentially intervene.
Notes
Funding statement
None
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: GM, AS. Study design: GM, AS. Methodology: GM, AS. Data collection: NA. Investigation: GM, AS. Statistical analysis: NA. Writing—original draft: GM. Writing—review & editing: GM, AS. Funding acquisition: NA. Approval of final manuscript: all authors.

